Open-Angle Glaucoma — August 2023 Archive
August 2023 at SpringMeds focused on one clear topic: open-angle glaucoma. We published a practical guide that explains what causes it, how it sneaks up on you, and the real treatment options you can discuss with your eye doctor.
What we covered
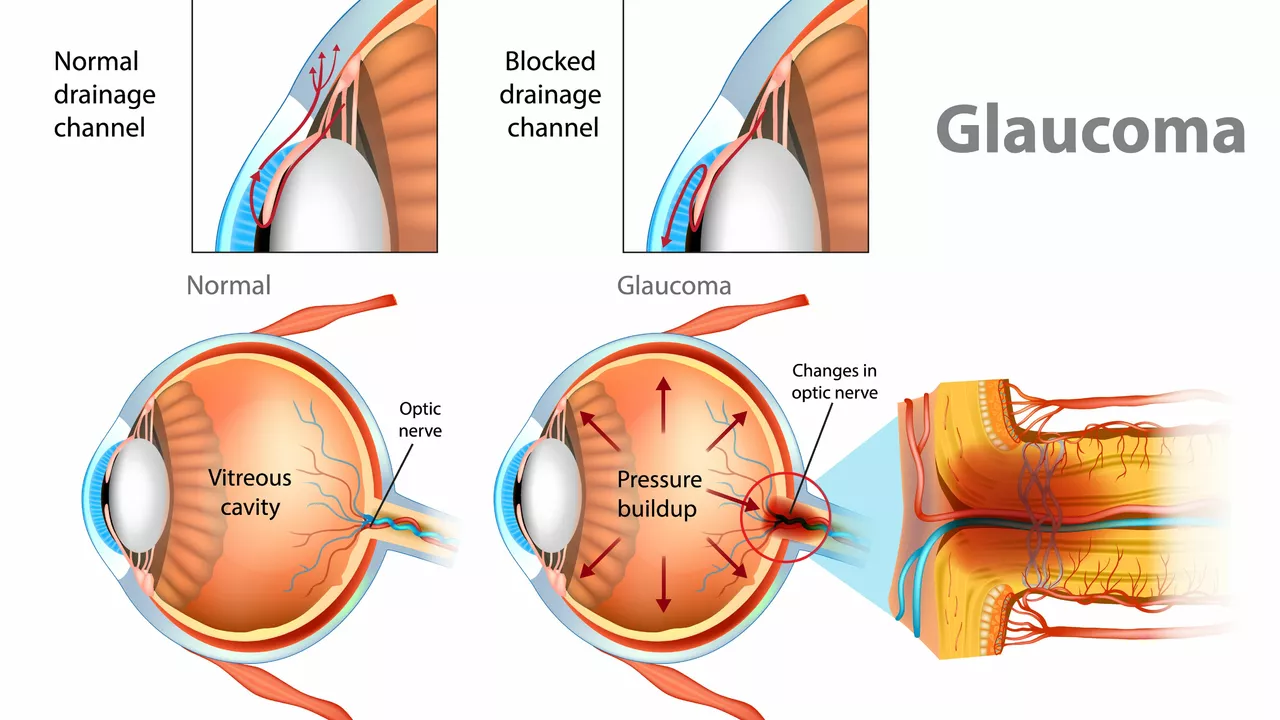
The post explains that open-angle glaucoma usually comes from blocked eye drainage channels that raise pressure inside the eye. Early on you often have no symptoms, but peripheral vision slowly fades before central sight is affected. We describe common risk factors like age over 40, family history, high eye pressure, diabetes, and certain ethnic backgrounds. Diagnosis steps are laid out simply: pressure check (tonometry), optic nerve exam, and visual field testing to spot early loss.
Treatment options are presented in plain terms. First-line therapy is usually daily eye drops that lower eye pressure. We explain how different drops work, common side effects to watch for, and why sticking to the schedule matters. If drops are not enough, laser trabeculoplasty is a quick clinic procedure that helps drainage. For more advanced cases, we cover surgical choices such as trabeculectomy and drainage implants, when they are considered, and what recovery looks like.
Quick action steps
If you have risk factors, book a comprehensive eye exam now and tell your doctor about any family history. If prescribed drops, set a daily reminder and keep a simple checklist so you do not skip doses. Bring up side effects—many can be managed or changed. Ask your eye doctor about laser options before jumping to surgery, and discuss follow-up schedules so progress is tracked with visual fields and nerve imaging.
We also give practical tips: store drops at recommended temperatures, avoid touching the bottle tip to your eye, and learn punctal occlusion (pressing the corner of the eye for a minute) to reduce systemic absorption. For people on multiple medications, ask if generic eye drops are safe and whether spacing times avoids interactions with other eye treatments.
Who should get checked earlier? If you have a close relative with glaucoma, are of African or Hispanic descent, have diabetes, take long-term steroid medications, or have had eye trauma, ask for a full glaucoma workup sooner than routine screenings. Typical follow-ups vary: newly diagnosed patients often return every three months until pressure and fields are stable; stable patients may move to six- or twelve-month visits. When talking to your doctor, ask for your target eye pressure, whether imaging of the optic nerve will be used to track change, and how quickly they expect to see improvement after new treatment. Finally, keep a simple eye diary noting vision changes, side effects, and missed doses so appointments are focused and effective.
Read the full post for a friendly, no-nonsense walkthrough of causes, signs, and treatment paths. Whether you are worried about early changes or managing a diagnosis, the August 2023 article gives straightforward steps you can take with your doctor to protect vision and plan care that fits your life.
Stay proactive today.