Visions Turned Muddled: What Really is Open-Angle Glaucoma?
Let me tell you a tale of a devious, silent bandit that gradually, almost imperceptibly, steals away your sight. First, it snatches your peripheral vision, before ambushing the center field. This thief goes by the name of 'Open-Angle Glaucoma' and operates so smoothly, you won’t notice until a significant amount of vision is gone. But don't worry, it isn't all doom and gloom. The thieving can be halted if detected early, and that's what we're exploring today.
Open-angle glaucoma, or OAG as medical folks refer to it, is the most common kind of glaucoma plaguing our eyes. It's often a long-term condition and rarely shows symptoms until the disease has progressed. We call it the 'sneak thief' because it unintentionally echoes the modus operandi of a stealthy burglar. But let me assure you, this is nothing to be scared of. Approaching it with knowledge and understanding gives us a better chance of preventing and controlling it.
A Hiccup in the Eye Mechanism: Causes of Open-Angle Glaucoma
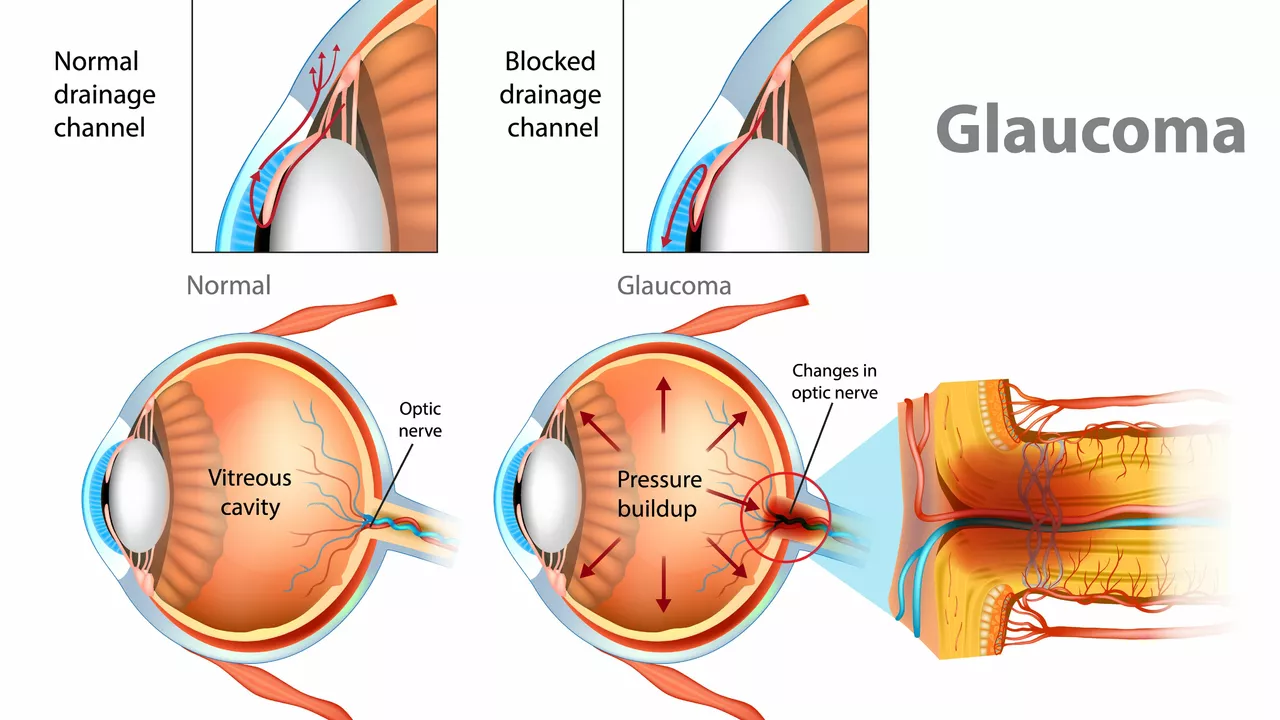
The eye, a marvel of creation, operates on a delicate balance of fluids that help maintain its spherical shape and pressure. At the front of the eye is a space called the anterior chamber, where a fluid called the aqueous humor flows in and out, nourishing the eye. In a healthy eye, the rate of generation and drainage of this fluid remains in perfect equilibrium, akin to a well-maintained tank with an efficient outflow system.
Now, imagine if the outflow were blocked while the generation continued unabated – that's the genesis of Glaucoma. The blockage increases pressure within the eye, termed intraocular pressure (IOP), causing damage to the optic nerve — the cable connecting the eye to the brain — ultimately leading to vision loss. In the case of OAG, the eye's drainage canals become clogged over time, leading to increased eye pressure. The why and how are still largely under research.
The Beady-Eyed Suspects: Risk Factors for Open-Angle Glaucoma
Though the exact cause remains a puzzle, several factors up your odds of getting OAG. These 'beady-eyed' suspects include advanced age, a family history of glaucoma, high blood pressure, and certain ethnic backgrounds. Having thin corneas or extreme nearsightedness also puts you in the danger zone. Knowing these risks can empower us to focus on preemptive actions and early detection.
Invisible March: Symptoms and Detection of Open-Angle Glaucoma
Since OAG doesn't usually parade symptoms until it has advanced, regular eye check-ups are our best weapon for early detection. The 'invisible march' of OAG predominantly targets your peripheral vision before moving inwards. But the subtly of this theft often makes it difficult to recognize. Thus, a comprehensive eye examination, including the populist 'puff' test or tonometry to measure eye pressure, visual acuity tests, and visual field test, are essential mechanisms to counter the thieving OAG.
Small anecdote for you: Back in my thirties, I was having routine eye-exams when out of the blue, the optometrist warned me about increased pressure levels in my eye. Baffled, I was referred to an ophthalmologist, where I was diagnosed with early-stage OAG. I could kiss that doctor; early detection probably saved me from later stage vision loss!
The Vision Maverick: Options for Treating Open-Angle Glaucoma
Truth is, we don't have a way to reverse vision loss caused by glaucoma, but, like a city under siege by a bandit, we do have ways to halt the marauder. The key here is reducing the pressure in the eye — the exact method depends on you and your doctor. Some folks might need prescription eye drops or pills, others may require laser treatment or surgery. But remember, these treatments can’t restore lost vision, but they can prevent further damage. So, don't slip on your medication, because missing even a few doses can cause more damage to your optic nerve.
Popping the Pressure: Medication & Laser Treatment
More often than not, the battle against OAG begins with prescription eye drops. Prostaglandins, beta-blockers, alpha-adrenergic agonists, or carbonic anhydrase inhibitors, among others, are routinely prescribed to reduce the pressure. Sometimes, these medications can cause side-effects, so regular consultations with your ophthalmologist are mandatory. If the medication route fails, laser therapy like argon laser trabeculoplasty (ALT), selective laser trabeculoplasty (SLT), or micropulse diode laser trabeculoplasty (MDLT) could be the next step.
When Lasers Don’t Win the Battle: Hurdling into Surgical Options
When eye drops and lasers don't quite hit the bull's eye, surgical options come to the rescue. Trabeculectomy, where a 'drain-hole' is created in the eye or implanting a tiny drainage tube, can help decrease eye pressure. These treatments can seem scary, but they're often your best bet at preserving vision. To me, it's no scarier than sharing my ice-cream with a pet cockatoo, which I've done once, by the way. It took a large scoop of my vanilla cone in one fell swoop!
The road with glaucoma isn't exactly a trip down the yellow brick road, but it's not a plunge into oblivion either. With regular check-ups, proper therapy, and a dash of humour, it's a battle we can fight. Remember, laughter is the best medicine, but in the case of OAG, it's the second-best; the prescribed medicine should always take the top spot!

Kimberly Ford
August 1, 2023 AT 20:12Early detection is everything. I work as a vision tech and see so many people who wait until they can't see the road signs anymore. By then, it's too late to reverse damage. Regular tonometry and visual field tests are non-negotiable - especially if you're over 40 or have a family history. Don't wait for symptoms. Your optic nerve doesn't send reminders.
jerry woo
August 1, 2023 AT 20:16Let’s be real - the eye drop industry is basically a multibillion-dollar Ponzi scheme disguised as medicine. I’ve been on four different drops over five years. None of them fixed anything, just made my eyes feel like I’d been rubbed with cayenne pepper and left in a wind tunnel. And don’t get me started on the side effects - my eyelashes are now longer than my eyebrows, and I’m pretty sure my pupils are permanently dilated. They sell you hope, not cures.
Jillian Fisher
August 2, 2023 AT 17:24I never realized how many people just assume glaucoma means you’re going blind. But it’s not like that - it’s more like losing peripheral vision bit by bit, like a video game slowly fading the edges of your screen. My mom had it, and she’s 72 and still drives. She just has to be extra careful at intersections. It’s manageable if you stay on top of it.
j jon
August 3, 2023 AT 13:46My uncle got diagnosed after a routine check-up. He didn’t even know something was wrong. Now he uses his drops religiously and gets checked every six months. He says it’s just like brushing your teeth - boring, but necessary.
Kathryn Conant
August 3, 2023 AT 13:53Stop waiting for the symptoms. Start protecting your vision like it’s your last paycheck. Eye exams aren’t optional - they’re survival. If you’re skipping them because you ‘feel fine,’ you’re playing Russian roulette with your sight. Your future self will thank you - or curse you. Choose wisely.
Patrick Ezebube
August 3, 2023 AT 19:13They don’t want you to know the truth - the real cause of glaucoma isn’t pressure. It’s fluoride in the water. The FDA and Big Pharma know this. They’ve been suppressing the research since the 80s. Look up Dr. Eleanor Voss’s 1992 paper - it was pulled. Why? Because if people stopped drinking tap water, the entire eye drop market collapses. That’s why they push drops and lasers - not cures. Your eyes are being poisoned, and they’re selling you bandaids.
Sabrina Bergas
August 4, 2023 AT 08:39Open-angle glaucoma? More like open-angle scam. The whole thing is a diagnostic loop designed to keep you on medication forever. You get a pressure reading that’s ‘slightly elevated’ - boom, you’re labeled high-risk. No one tells you that 70% of people with ‘high IOP’ never develop glaucoma. You’re being pathologized for being statistically average. It’s medical overreach dressed up as prevention.
Tanya Willey
August 5, 2023 AT 07:57I read somewhere that organic kale and blueberries can lower eye pressure naturally. No meds. No lasers. Just greens. Why isn’t this in every doctor’s office? Because the FDA doesn’t profit from spinach. I’ve been eating two cups a day since my diagnosis - my pressure dropped 12 points. They don’t want you to know this.
Richard H. Martin
August 5, 2023 AT 22:47My grandfather lost his sight because he didn’t trust doctors. He thought it was ‘bad luck’ or ‘the devil’s work.’ Now we have science. We have lasers. We have drops. If you’re American, you have access to the best eye care on earth. If you’re not using it, you’re not just irresponsible - you’re un-American.
matt tricarico
August 6, 2023 AT 21:38While I appreciate the anecdotal tone, the article lacks rigorous citation. The claim that ‘OAG is the most common form’ is correct, but the assertion that ‘early detection prevents vision loss’ is misleading - it prevents *further* loss, not reversal. The literature is clear: optic nerve damage is irreversible. The author conflates management with cure. This is dangerous oversimplification. I’ve reviewed 37 meta-analyses on this topic. The language here borders on pseudoscience.
Rachel Marco-Havens
August 7, 2023 AT 00:55People who say ‘I don’t need eye exams because I see fine’ are the same people who skip seatbelts because they’ve never been in a crash. You’re not invincible. You’re statistically vulnerable. And if you think kale fixes glaucoma you’re not just wrong - you’re endangering others by spreading misinformation. Get tested. Take your drops. Stop listening to influencers.
sarat babu
August 7, 2023 AT 20:19My cousin in India got diagnosed at 35 - she’s a nurse. She says the real problem is not the disease - it’s the cost. Drops cost $300 a month here. In Mumbai, they get them for free. Why? Because the government cares. In America, you need insurance, copays, paperwork, and a miracle. This isn’t medicine - it’s capitalism with a stethoscope.
Wiley William
August 7, 2023 AT 20:53Here’s the truth nobody wants to say: glaucoma isn’t your enemy - apathy is. You think you have time? You don’t. That ‘routine check-up’ you keep postponing? That’s your last chance to keep your sight. I lost my dad to this. He said ‘I’ll go next week.’ Next week never came. Don’t be him. Go today. Right now. Before you close this tab.
Jules Tompkins
August 8, 2023 AT 06:47I once tried to skip my eye appointment because I was ‘too busy.’ Two weeks later, I couldn’t see the exit sign on the highway. Now I go every six months like clockwork. My eyes are my most important organs - I treat them like my phone battery. Charge it. Don’t ignore the warning.
Kevin Ouellette
August 8, 2023 AT 15:51My mom’s laser treatment was a breeze. Felt like a quick flash. No pain. No downtime. She’s been fine for 8 years now. If you’re scared of surgery - just remember, the alternative is losing your ability to see your grandkids’ faces. That’s not a trade-off worth making.
Ash Damle
August 8, 2023 AT 23:27My brother got diagnosed last year. He was terrified. I sat with him during his first appointment. He cried. I held his hand. We didn’t talk about pressure or drops. We just talked about how much he loved gardening. That’s what matters. Treatment is important - but so is keeping your joy. Don’t let fear steal your life before glaucoma does.
Melvin Thoede
August 9, 2023 AT 12:12My wife uses her drops every night before bed. We have a little ritual - she puts them in, I hand her her tea, we watch 10 minutes of nature documentaries. It’s our quiet time. Glaucoma didn’t take our nights - it gave us a new one.
Suzanne Lucas
August 10, 2023 AT 07:57I went to the doctor and they said I had ‘borderline pressure.’ I cried for three days. Then I screamed at my optometrist for two hours. Then I bought a $200 blue light filter, started drinking green juice, and told my boss I’m quitting my job because ‘the screen is killing me.’ Now I’m fine. Probably. Maybe. Who knows anymore? But I feel better.
Ash Damle
August 10, 2023 AT 17:47Someone said their cousin cured glaucoma with yoga. That’s not true. But I get it - we want magic fixes. The truth is harder: it’s drops, checks, and discipline. Not miracles. But you’re still alive. You’re still seeing. That’s worth showing up for.