It’s 2026, and vaping still feels normal-especially to young adults who’ve never smoked a cigarette. You see it on the street, in movies, even in ads that make it look like a harmless habit. But here’s the truth: vaping isn’t just a safer alternative to smoking. It’s a direct, daily assault on your lungs, and the science is no longer whispering-it’s shouting.
What’s Actually in Vaping Aerosol?
Most people think e-cigarettes just produce water vapor. They don’t. What you’re inhaling is a fine mist of chemicals, many of which are known to damage lung tissue. The base liquids-propylene glycol and vegetable glycerin-sound harmless, but when heated and turned into aerosol, they break down into toxic compounds like acetaldehyde and formaldehyde. A University of North Carolina study found that the more ingredients in an e-liquid, the more toxic the vapor becomes. Flavors aren’t just for taste; they’re chemical bombs. Diacetyl, once used in microwave popcorn and linked to ‘popcorn lung,’ has been banned in many countries, but other flavoring agents like acetoin and pentanedione are still in use and behave the same way.
And it’s not just flavorings. Vaping devices release heavy metals-nickel, tin, lead-from the heating coils. Benzene, a known carcinogen found in car exhaust, shows up in vape aerosol too. The American Lung Association says these chemicals cause inflammation, cell death, and DNA damage. Even if you’re not smoking tobacco, you’re still exposing your lungs to substances that belong in a factory, not your airways.
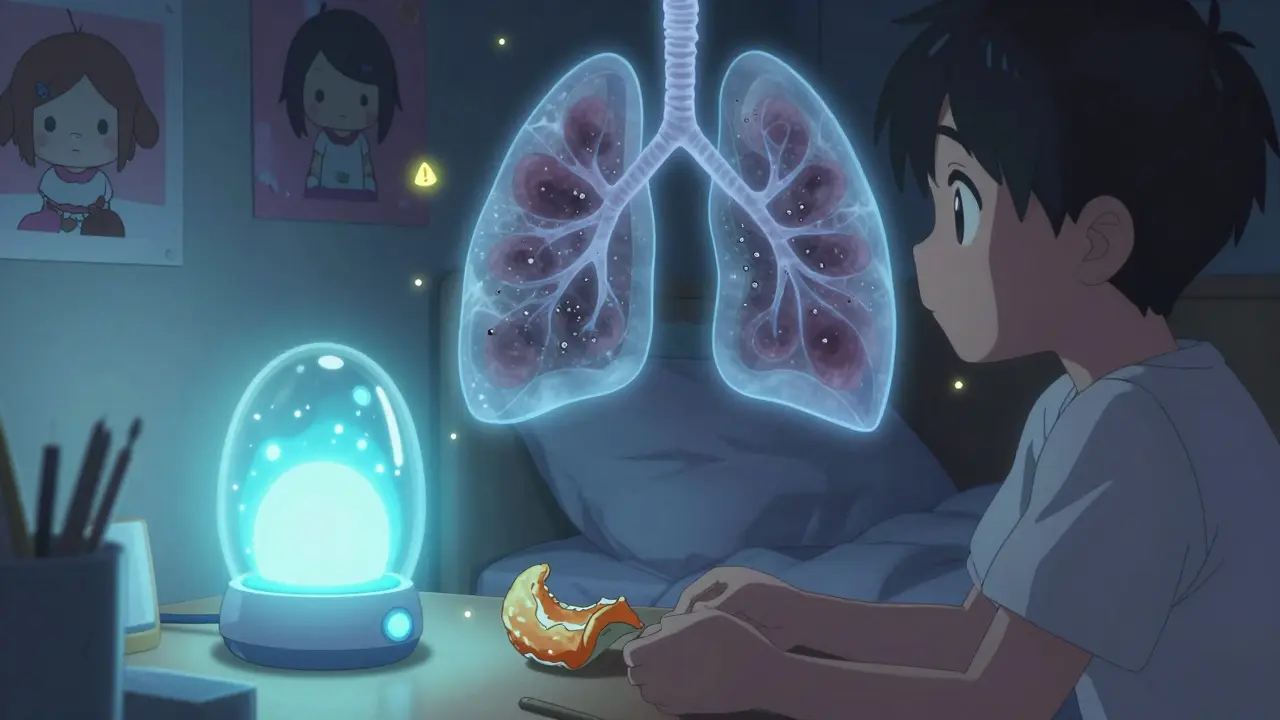
How Vaping Harms Your Lungs
Your lungs aren’t designed to handle chemical vapor. Every puff triggers inflammation. Studies show that even short-term vaping increases markers of lung inflammation in people with no prior respiratory issues. This isn’t just a cough or throat irritation-it’s your immune system reacting to foreign toxins. Over time, this constant irritation leads to scarring, thickened airway walls, and reduced lung capacity.
The biggest danger? Your lungs lose their ability to fight off infection. Research from the American Thoracic Society found that e-cigarette vapor suppresses alveolar macrophages-the cells that clear bacteria and debris from your lungs. This means vapers are more likely to get pneumonia, bronchitis, and even severe flu complications. One 2024 study showed vapers had a 30% higher risk of respiratory infections than non-users, even after adjusting for smoking history.
And then there’s COPD. Chronic Obstructive Pulmonary Disease used to be a smoker’s disease. Now, it’s showing up in people in their 30s who’ve never lit a cigarette. A major NIH analysis of over 100,000 adults found that current e-cigarette users had a 48% higher risk of developing COPD compared to non-users. That’s not a small increase. That’s a clear signal: vaping isn’t just risky-it’s accelerating lung disease.
The EVALI Crisis Wasn’t a Fluke
In 2019, over 2,800 people in the U.S. were hospitalized with a mysterious lung illness linked to vaping. Forty-seven died. The cause? Vitamin E acetate, a thickening agent used in black-market THC vape cartridges. It wasn’t nicotine. It wasn’t flavoring. It was a cosmetic additive turned poison in the lungs.
What most people don’t realize is that EVALI wasn’t an accident-it was a warning. The system failed. Unregulated products flooded the market. People thought they were safe because they weren’t smoking tobacco. But the lungs don’t care if the toxin comes from a legal store or a street dealer. They only care if it’s inhaled. Even now, with tighter regulations, black-market vapes still circulate. And the ingredients? Many aren’t tested. Not by the FDA. Not by anyone.
Is Vaping Better Than Smoking?
Yes, if you’re a current smoker and you switch completely to vaping, you’ll reduce your exposure to tar and thousands of other carcinogens found in tobacco smoke. That’s why some health groups say vaping is ‘less harmful.’ But ‘less harmful’ doesn’t mean ‘harmless.’
Here’s the problem: most people who vape don’t quit smoking-they do both. Dual use is common. And when you combine the toxins from cigarettes and vapes, your lung damage multiplies. Worse, many young vapers have never smoked. They’re starting with vaping and then moving to cigarettes. The National Academies found that teens who vape are three times more likely to start smoking within a year.
And if you’re using vaping to quit smoking? The evidence is mixed. Some people succeed. Many don’t. And the lung damage from vaping continues regardless of your original goal. The safest path isn’t swapping one habit for another-it’s quitting nicotine entirely.
What Symptoms Should You Watch For?
You don’t need to be hospitalized to have lung damage. The early signs are quiet:
- A persistent cough that won’t go away
- Shortness of breath during light activity-like walking up stairs
- Chest tightness or pain
- Frequent bronchitis or pneumonia
- Decreased ability to exercise or stay active
These symptoms often get dismissed as ‘just allergies’ or ‘getting out of shape.’ But if you vape and you’re experiencing any of these-even mildly-it’s not normal. It’s your body telling you something’s wrong. Lyracore’s 2025 report recommends anyone with these symptoms, especially under 40, get evaluated by a pulmonary specialist. Early detection can prevent irreversible damage.

Can Your Lungs Heal After Quitting?
Yes-but only if you stop. The good news? Inflammation starts to drop within weeks. Lung function can improve in as little as 3 to 6 months after quitting. Studies show that former vapers who stop for a year see measurable improvements in airway resistance and cough frequency.
But here’s the catch: some damage may be permanent. Scarring in the lung tissue, changes to immune cell function, and altered gene expression in lung cells don’t always reverse. The longer you vape, the less likely full recovery becomes. Think of it like sun exposure-some redness fades, but wrinkles and DNA damage stick around.
There’s no magic pill. No supplement. No detox tea. The only proven way to protect your lungs is to stop vaping. Completely. And if you’re struggling to quit, talk to a doctor. Nicotine replacement therapy, counseling, and even prescription medications like varenicline have been shown to work better than trying to quit cold turkey.
What’s Next for Vaping and Public Health?
The vaping industry is growing, and so are the lawsuits. Regulators are finally catching up-Australia banned flavored vapes in 2024, the UK is tightening advertising rules, and the U.S. FDA is cracking down on unapproved products. But enforcement is slow. The market is still flooded with cheap, unregulated devices that can explode from faulty batteries or leak toxic chemicals.
The real challenge? Youth. Vaping rates among teens have dropped since 2020, but they’re still far too high. And now, companies are marketing nicotine pouches and discreet pod devices that look like USB drives. Kids aren’t vaping to quit smoking. They’re vaping because it’s cool, flavored, and easy to hide.
The science is clear: vaping isn’t a solution. It’s a new public health crisis in slow motion. We’re seeing the same patterns we saw with cigarettes 50 years ago-denial, delayed action, and a generation paying the price.
Does vaping cause lung cancer?
There’s no direct evidence yet that vaping causes lung cancer in humans, but it’s not because it’s safe. The problem is that vaping hasn’t been around long enough. We’re still waiting for 20- to 30-year studies. What we do know is that vaping exposes the lungs to carcinogens like formaldehyde and acrolein-substances proven to damage DNA and cause cancer in animal studies. The American Cancer Society says it’s too early to rule out cancer risk, and we should treat vaping like a potential threat, not a harmless habit.
Are nicotine-free vapes safe?
No. Even nicotine-free vapes contain the same toxic base chemicals-propylene glycol, vegetable glycerin, and flavoring agents. Studies show these alone can cause airway inflammation and cell damage. The nicotine isn’t the only problem. The act of inhaling heated chemicals into your lungs is the core risk. If you think nicotine-free means safe, you’re mistaken.
Can vaping affect my asthma?
Yes, badly. The National Academies of Science found strong evidence that vaping increases asthma attacks in teens and adults. The chemicals in vape aerosol irritate the airways, making them more sensitive and prone to swelling. People with asthma who vape report more emergency room visits, more steroid use, and worse control of their symptoms. If you have asthma, vaping makes it harder to manage-and more likely to become life-threatening.
Is secondhand vape aerosol dangerous?
Absolutely. The U.S. Surgeon General confirmed that secondhand vape aerosol contains nicotine, ultrafine particles, and toxic chemicals like formaldehyde and heavy metals. Children exposed to vape aerosol have higher rates of respiratory infections and wheezing. There’s no safe level of exposure. If you vape around others, you’re putting them at risk-even if they don’t vape themselves.
What should I do if I vape and feel short of breath?
Stop vaping immediately and see a doctor. Don’t wait. Shortness of breath isn’t something you should ignore-it’s a red flag. Get a lung function test (spirometry) and ask for a chest X-ray or CT scan if symptoms persist. Many people assume it’s just a cold or allergies, but if you vape, your lungs are already under stress. Early intervention can prevent permanent damage.
Final Thought: Your Lungs Don’t Lie
They don’t care if it’s called a vape, an e-cig, or a pod. They don’t care if it’s flavored with mango or menthol. They don’t care if you think it’s safer than cigarettes. Your lungs only respond to what’s in the air you breathe-and vaping is filling that air with chemicals your body wasn’t built to handle.
If you’re vaping now, the best thing you can do is quit. Not tomorrow. Not next month. Now. Your lungs will thank you. And if you’re not vaping but thinking about it? Don’t start. There’s no upside that outweighs the risk. The evidence isn’t debatable anymore. It’s here. It’s clear. And it’s written in your lungs.


ellen adamina
January 17, 2026 AT 10:02My lungs have been fine since I quit last year. No cough. No wheezing. Just breathe.
Jami Reynolds
January 18, 2026 AT 06:08Let’s be honest-this is all part of the Great Vaping Cover-Up. The FDA, Big Pharma, and the WHO have been suppressing studies since 2018 showing that vaping triggers a latent autoimmune cascade in the alveoli. The real danger isn’t the chemicals-it’s the silence. They don’t want you to know that vaping accelerates epigenetic silencing of lung repair genes. They’ve been doing this since tobacco. Always the same playbook.
Tom Doan
January 18, 2026 AT 22:12So let me get this straight: you’re telling me that inhaling heated glycerin is worse than inhaling tar-laced smoke from a 2,000-year-old plant? And yet, we’re supposed to believe the ‘science’ that says vaping is ‘just as bad’? I’d like to see the double-blind, placebo-controlled trial where they compared 10-year vapers to non-users with identical genetic backgrounds, socioeconomic status, and air quality exposure. Oh wait-we can’t. Because the science isn’t science. It’s advocacy dressed in lab coats.
Sohan Jindal
January 19, 2026 AT 06:27They’re trying to take away our freedom. You think this is about health? No. It’s about control. The government wants you dependent on their nicotine patches and their counseling programs. They don’t want you making your own choices. Vaping saved me from cigarettes. Now they want to ban it because they hate people who think for themselves.
RUTH DE OLIVEIRA ALVES
January 20, 2026 AT 18:45While the article presents a compelling synthesis of current biomedical literature, it is imperative to acknowledge the epistemological limitations inherent in longitudinal observational studies, particularly those reliant on self-reported behavioral data. The conflation of correlation with causation, especially in the context of multifactorial pulmonary pathologies, warrants a more nuanced interpretive framework. Furthermore, the rhetorical framing of vaping as an ‘assault’ risks pathologizing personal autonomy under the guise of public health imperatives.
Gloria Montero Puertas
January 22, 2026 AT 00:08Oh, please. You think you’re being ‘honest’? You’re just another middle-class, overeducated, guilt-ridden American who thinks breathing is a moral obligation. You’ve never even held a vape pen, have you? You’re terrified of people who enjoy flavor, who choose something ‘less bad’-and you punish them with fearmongering. Your ‘science’ is just your ego dressed in citations.
Frank Geurts
January 23, 2026 AT 20:24As a global public health professional with over two decades of fieldwork across five continents, I can affirm that the trajectory of nicotine delivery systems follows a predictable epidemiological arc: initial adoption, regulatory lag, delayed recognition of harm, and eventual policy correction. The United States’ current stance is neither reactionary nor alarmist-it is the inevitable culmination of decades of precedent. What distinguishes this moment is the unprecedented scale of youth exposure, coupled with the commercialization of aerosolized neurotoxins under the guise of lifestyle enhancement. This is not a debate. It is a historical inflection point.
Niki Van den Bossche
January 24, 2026 AT 07:14There’s a poetry to it, really-the human body, a cathedral of evolution, forced to inhale the ghost of a factory’s waste stream, flavored like a child’s birthday cake. We’ve turned the sacred act of breathing into a consumer product, a dopamine-delivery system wrapped in plastic and marketed with neon. We’re not just vaping-we’re performing a ritual of self-erasure, one puff at a time. The lungs don’t scream. They just… stop.
Arjun Seth
January 24, 2026 AT 09:43Why do you think they push this? It’s not about health. It’s about money. Big Pharma makes billions from asthma inhalers, COPD meds, and lung cancer treatments. If people stop vaping, they stop getting sick. Then who pays for their drugs? They need you sick. Always. That’s the truth. They want you to think it’s science. It’s profit.
Haley Graves
January 26, 2026 AT 01:36You don’t have to be perfect to make a change. If you’re vaping and you’re worried-stop. Don’t wait for permission. Don’t wait for the perfect plan. Just stop. One day at a time. Talk to someone. Try a patch. Call a quitline. You don’t have to be a hero. You just have to be done. Your lungs are already trying to heal. Give them a chance.
Crystel Ann
January 26, 2026 AT 19:17I used to vape daily. Then I started getting winded walking to my mailbox. I quit cold turkey in January. Three months later, I hiked 5 miles with my niece. She didn’t even know I’d ever vaped. It wasn’t magic. It was just… breathing again.
Mike Berrange
January 27, 2026 AT 15:46Interesting how the article cites studies from institutions that receive funding from tobacco control coalitions. Meanwhile, the 2023 UK Health Security Agency report found no significant increase in COPD incidence among exclusive vapers over five years. But of course, that doesn’t fit the narrative. The truth is inconvenient when your moral outrage is the product you’re selling.