Introduction to Pancreatic Cancer and Immunotherapy
Pancreatic cancer is a devastating disease with a low survival rate, and finding effective treatment options has been a challenge for researchers and medical professionals alike. Immunotherapy, a relatively new approach to cancer treatment, has shown promise in treating various types of cancer. In this article, we'll explore the role of immunotherapy in pancreatic cancer treatment and dive into the different strategies being utilized to combat this deadly disease. We'll also discuss the potential benefits and drawbacks of incorporating immunotherapy in the fight against pancreatic cancer.
Understanding Pancreatic Cancer
Pancreatic cancer occurs when malignant cells develop in the pancreas, an essential organ that plays a crucial role in digestion and blood sugar regulation. The most common type of pancreatic cancer is adenocarcinoma, which arises from the pancreatic ducts. Pancreatic cancer is often aggressive and difficult to treat, mainly because it is frequently diagnosed at an advanced stage. Symptoms often appear late, and the cancer spreads quickly to surrounding areas, making surgical removal challenging.
Traditional treatment options for pancreatic cancer include surgery, chemotherapy, and radiation therapy. Unfortunately, these treatments alone have not been sufficient in improving survival rates for patients with advanced pancreatic cancer. This has led researchers to search for innovative treatment approaches, such as immunotherapy, to boost the body's immune system and fight the cancer more effectively.
What is Immunotherapy?
Immunotherapy is a type of cancer treatment that uses the body's own immune system to identify, attack, and destroy cancer cells. The immune system is a complex network of cells, tissues, and organs that work together to defend the body against harmful invaders like bacteria, viruses, and cancerous cells. Immunotherapy treatments aim to either enhance the immune system's natural ability to fight cancer or provide it with additional tools to target and destroy cancer cells.
There are several types of immunotherapy, including checkpoint inhibitors, cancer vaccines, adoptive cell transfer, and oncolytic viruses. These therapies have shown promising results in treating different types of cancer, including melanoma, lung cancer, and kidney cancer. However, the role of immunotherapy in pancreatic cancer treatment is still under investigation.
Checkpoint Inhibitors and Pancreatic Cancer
Checkpoint inhibitors are a type of immunotherapy that targets specific proteins on the surface of cancer cells or immune cells. These proteins act as "brakes" on the immune system, preventing it from attacking healthy cells. By blocking these proteins, checkpoint inhibitors can "release the brakes" and enable the immune system to recognize and attack cancer cells more effectively.
In some cancer types, checkpoint inhibitors have shown significant success in improving survival rates. However, in pancreatic cancer, the results have been less promising, possibly due to the unique immunosuppressive environment surrounding pancreatic tumors. Researchers are working to identify potential biomarkers that could help predict which patients may benefit from checkpoint inhibitors or develop combination therapies to enhance their effectiveness in pancreatic cancer treatment.
Cancer Vaccines for Pancreatic Cancer
Cancer vaccines are another type of immunotherapy that aims to stimulate the immune system to recognize and attack cancer cells. These vaccines often contain cancer-specific proteins or antigens that activate the immune system's T cells, enabling them to target and destroy cancer cells. Some cancer vaccines are designed to prevent specific types of cancer, while others are used to treat existing cancers.
Several cancer vaccines are being investigated for their potential in treating pancreatic cancer. One example is GVAX, a vaccine made from genetically modified pancreatic cancer cells that produce an immune-stimulating protein called GM-CSF. Early clinical trials have shown some promising results, but further research is needed to determine the effectiveness and safety of cancer vaccines in pancreatic cancer treatment.
Adoptive Cell Transfer and Pancreatic Cancer
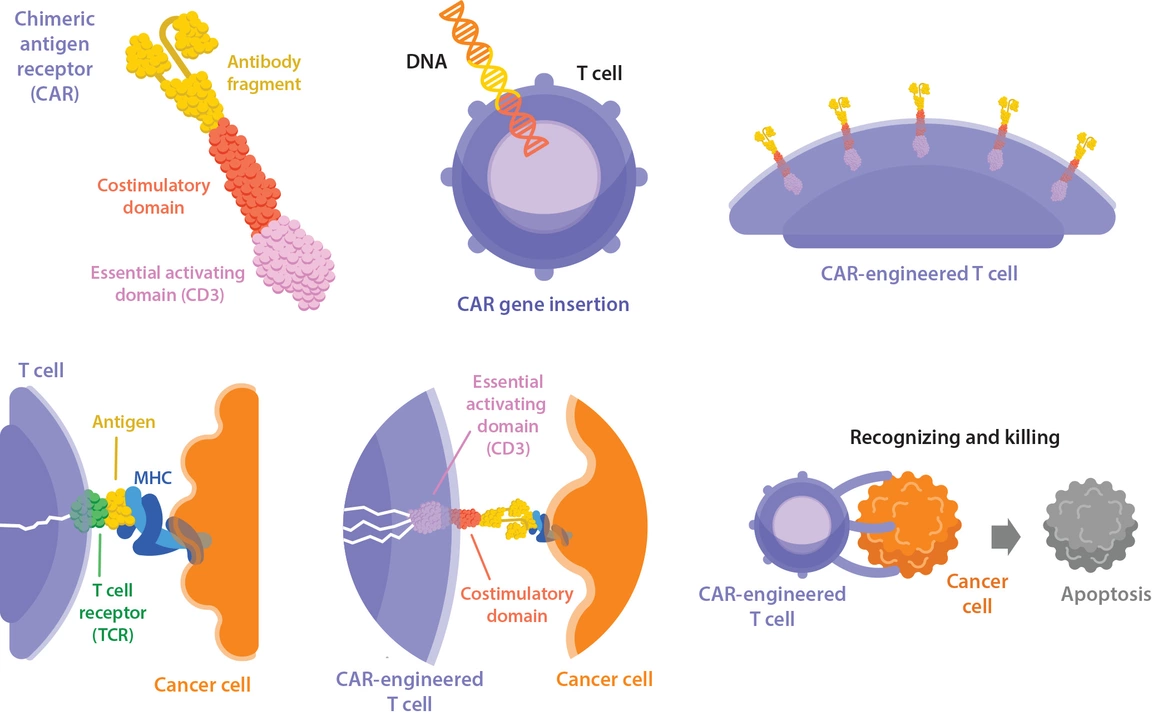
Adoptive cell transfer is an innovative immunotherapy approach that involves collecting a patient's immune cells, modifying them to better target cancer cells, and then infusing them back into the patient. One form of adoptive cell transfer, known as chimeric antigen receptor (CAR) T-cell therapy, has shown remarkable success in treating certain blood cancers like leukemia and lymphoma.
Researchers are now exploring the potential of adoptive cell transfer for treating solid tumors, including pancreatic cancer. However, there are several challenges to overcome, such as identifying suitable targets on pancreatic cancer cells and ensuring that the modified immune cells can effectively infiltrate the tumor environment. While still in the early stages of development, adoptive cell transfer offers a promising avenue for future pancreatic cancer treatment strategies.
Oncolytic Viruses and Pancreatic Cancer
Oncolytic viruses are another type of immunotherapy that uses modified viruses to infect and destroy cancer cells. These viruses are engineered to selectively target cancer cells, leaving healthy cells unharmed. Once inside the cancer cells, the viruses replicate and cause the cells to burst, releasing more viruses to continue the process. Additionally, the destruction of cancer cells can stimulate the immune system to mount a more robust response against the remaining tumor cells.
Several oncolytic viruses are being investigated for their potential in treating pancreatic cancer, including modified versions of the measles virus and the herpes simplex virus. Early clinical trials have shown some promising results, but further research is needed to determine the optimal way to deliver the viruses and how to combine them with other treatments for the best outcomes.
Combination Therapies for Pancreatic Cancer
One of the most promising strategies for using immunotherapy in pancreatic cancer treatment is combining it with other treatments, such as chemotherapy, radiation therapy, or targeted therapies. The rationale behind combining treatments is that they may work together to enhance the effectiveness of each therapy, target different aspects of the cancer, and potentially overcome the immunosuppressive environment of pancreatic tumors.
Several clinical trials are currently underway to investigate the potential of combination therapies in treating pancreatic cancer. These trials aim to determine the most effective combinations, optimal treatment sequencing, and potential side effects or complications of combining different therapies.
Potential Benefits and Drawbacks of Immunotherapy for Pancreatic Cancer
Immunotherapy offers several potential benefits for pancreatic cancer treatment. By harnessing the power of the immune system, immunotherapy may provide a more targeted and effective approach to fighting cancer cells. Additionally, immunotherapy may offer longer-lasting protection against cancer recurrence, as the immune system can "remember" the cancer cells and mount a response if they reappear.
However, there are also potential drawbacks to using immunotherapy for pancreatic cancer. One significant challenge is the immunosuppressive environment of pancreatic tumors, which may limit the effectiveness of certain immunotherapies. Additionally, immunotherapy can cause various side effects, ranging from mild flu-like symptoms to severe autoimmune reactions. Finally, the cost of immunotherapy treatments can be quite high, potentially limiting accessibility for some patients.
Conclusion
While immunotherapy has shown promise in treating various types of cancer, its role in pancreatic cancer treatment is still under investigation. Researchers are exploring different immunotherapy strategies, such as checkpoint inhibitors, cancer vaccines, adoptive cell transfer, and oncolytic viruses, to determine their effectiveness in targeting pancreatic cancer cells. Additionally, combination therapies with chemotherapy, radiation therapy, or targeted therapies offer a promising approach to enhancing the potential benefits of immunotherapy in treating pancreatic cancer.
As research and clinical trials continue, we can remain hopeful that immunotherapy will play a more significant role in improving the prognosis and quality of life for pancreatic cancer patients in the future.

jennifer sizemore
April 30, 2023 AT 04:53jerry woo
April 30, 2023 AT 19:14Kimberly Ford
May 1, 2023 AT 00:00Jillian Fisher
May 1, 2023 AT 14:52Kathryn Conant
May 1, 2023 AT 16:27Jules Tompkins
May 2, 2023 AT 09:43Sabrina Bergas
May 2, 2023 AT 15:54Patrick Ezebube
May 2, 2023 AT 21:44Armando Rodriguez
May 3, 2023 AT 01:40Kevin Ouellette
May 3, 2023 AT 07:02j jon
May 3, 2023 AT 09:38Ash Damle
May 3, 2023 AT 18:23Melvin Thoede
May 4, 2023 AT 16:12Rachel Marco-Havens
May 4, 2023 AT 21:01Suzanne Lucas
May 5, 2023 AT 12:04matt tricarico
May 5, 2023 AT 20:26