Antibiotic Selection Tool
Select Your Condition
Patient Factors
Recommended Antibiotics
Quick Takeaways
- Terramycin (tetracycline) is effective for many bacterial infections but has notable side‑effects and food interactions.
- Doxycycline and minocycline offer better GI tolerance and longer half‑life, making dosing easier.
- Azithromycin works well for atypical pathogens and has a short course, but resistance is rising.
- Amoxicillin remains the go‑to for many common infections, especially when beta‑lactam coverage is needed.
- Cost, local resistance patterns, and patient allergies decide which drug is best.
What Is Terramycin?
When people hear Terramycin, they are hearing the brand name for the broad‑spectrum antibiotic tetracycline. First approved in the 1950s, tetracycline fights a wide range of Gram‑positive and Gram‑negative bacteria by binding to the 30S ribosomal subunit, halting protein synthesis.
Because it’s an older drug, its manufacturing cost stays low, and it’s still stocked in many pharmacies across Australia, the UK, and the US.
How Terramycin Works (and Why It Matters)
By preventing bacteria from creating essential proteins, tetracycline stops them from multiplying. This mechanism makes it useful for acne, respiratory infections, chlamydia, and eye infections. However, the same binding site is also found in mitochondria, leading to side‑effects like photosensitivity and nausea when taken without food.
When Doctors Choose Terramycin
Typical indications include:
- Uncomplicated urinary tract infections caused by susceptible strains.
- Acute bacterial conjunctivitis.
- Rickettsial diseases such as RockyMountain spotted fever.
- Mild to moderate acne.
It’s rarely first‑line for severe pneumonia or infections where resistant organisms dominate.
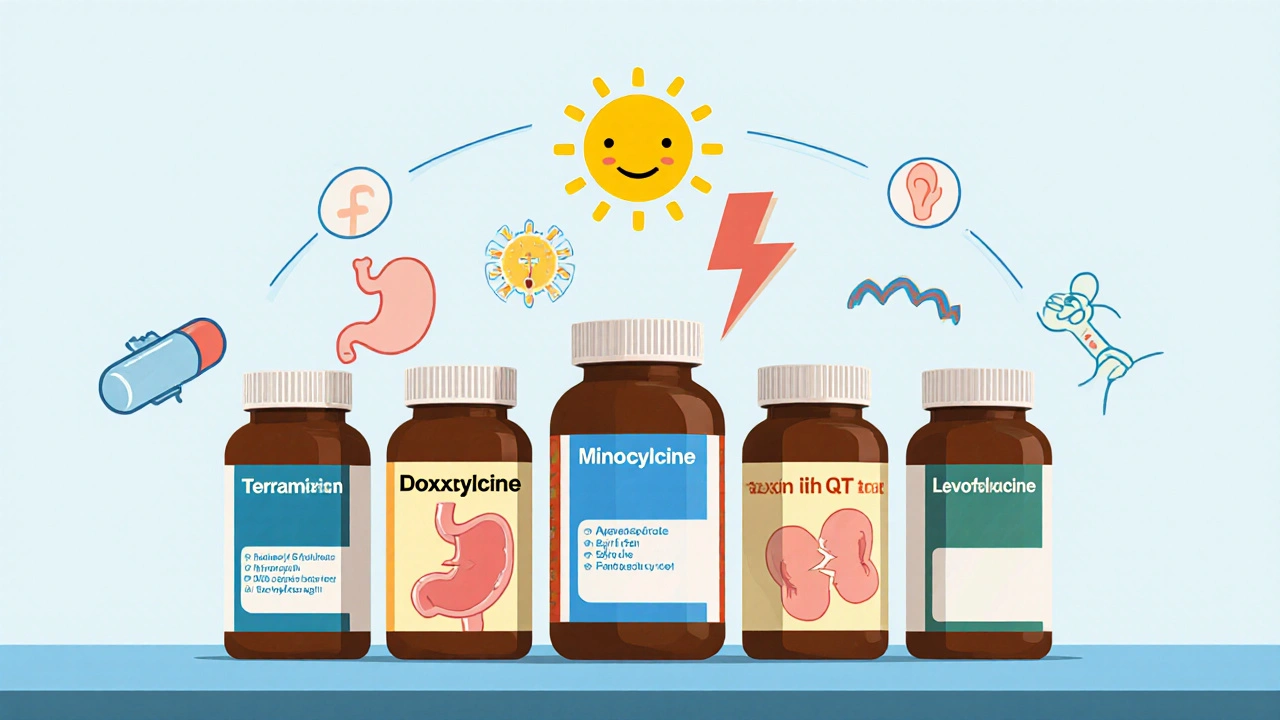
Alternatives on the Market
Below are the most common antibiotics that doctors compare to tetracycline when prescribing:
- Doxycycline - a second‑generation tetracycline with a longer half‑life.
- Minocycline - similar spectrum, less GI upset, but can cause vestibular side‑effects.
- Azithromycin - a macrolide with a short 5‑day course, good for atypical pathogens.
- Amoxicillin - a beta‑lactam ideal for many ear, nose, throat infections.
- Levofloxacin - a fluoroquinolone reserved for complicated cases.
Side‑Effect Profile: Terramycin vs. Its Peers
All antibiotics carry risks, but the pattern differs:
| Antibiotic | GI Upset | Photosensitivity | Resistance Concerns | Special Warnings |
|---|---|---|---|---|
| Terramycin (tetracycline) | Moderate | High | Increasing | Contraindicated in pregnancy, children <5yr |
| Doxycycline | Low | Moderate | Stable | Same pregnancy restrictions |
| Minocycline | Low | Low | Stable | Rare vestibular toxicity |
| Azithromycin | Low | Low | Rising in respiratory pathogens | QT prolongation risk |
| Amoxicillin | Low‑moderate | None | High in beta‑lactamase producers | Allergy in penicillin‑sensitive patients |
| Levofloxacin | Low | None | High selective pressure | Tendon rupture, CNS effects |

Choosing the Right Antibiotic for Your Situation
Here’s a quick decision guide you can use when you or a clinician is picking a drug:
- Identify the likely bug - Gram‑positive, Gram‑negative, atypical, or mixed.
- Check local resistance data - many Australian labs publish yearly antibiograms.
- Consider patient factors - age, pregnancy status, kidney function, drug allergies.
- Match the dosing schedule to adherence - once‑daily drugs (doxycycline, azithromycin) improve compliance.
- Factor in cost and insurance coverage - generic tetracycline is cheap, but doxycycline may be covered better under Medicare.
For example, a 30‑year‑old with uncomplicated chlamydia often receives doxycycline 100mg twice daily for seven days, because it’s easier on the stomach and requires fewer food restrictions than tetracycline.
If a patient has a severe acne flare and weighs under 50kg, minocycline at 50mg daily may be preferable, avoiding the high photosensitivity that would force the patient to stay indoors.
Cost & Availability in 2025
According to the Australian Pharmaceutical Benefits Scheme (PBS), a 14‑day course of generic tetracycline (Terramycin) costs roughly AUD6, while doxycycline is about AUD12. Azithromycin’s 5‑day pack averages AUD18, and levofloxacin sits near AUD30.
All six antibiotics are listed on major online pharmacy platforms in Australia, but some require a prescription - especially the fluoroquinolones and minocycline.
Practical Tips When Taking These Drugs
- Never take tetracycline or doxycycline with dairy or antacids; calcium binds the drug and cuts absorption by up to 70%.
- Wear sunscreen and protective clothing if you’re on any tetracycline‑class drug - photosensitivity can cause severe sunburn.
- Complete the full course even if symptoms improve; stopping early fuels antibiotic resistance, a trend the WHO flagged as a top global health threat.
- If you notice sudden joint pain while on levofloxacin, stop the medication and contact a clinician - tendon rupture, though rare, is a serious side‑effect.
- For children under eight, avoid tetracyclines entirely; they can cause permanent tooth discoloration.
Frequently Asked Questions
Is Terramycin still effective against modern bacterial strains?
Effectiveness varies by region. In Australia, recent surveillance shows 78% susceptibility for uncomplicated urinary pathogens, but resistance is climbing among Staphylococcus aureus. Always ask your lab for the latest antibiogram.
Can I switch from Terramycin to doxycycline without consulting a doctor?
Both drugs belong to the tetracycline class, but dosing schedules differ. Changing without medical guidance can lead to under‑dosing or unnecessary side‑effects. Talk to a pharmacist or prescriber first.
Why does Terramycin cause a metallic taste?
Tetracyclines can chelate metal ions in saliva, creating a temporary metallic sensation. Staying well‑hydrated and rinsing the mouth after each dose usually eases the feeling.
Is it safe to use Terramycin during pregnancy?
No. Tetracyclines cross the placenta and can cause fetal bone growth inhibition and tooth discoloration. Preferred alternatives in pregnancy include amoxicillin or azithromycin, depending on the infection.
How long does it take for photosensitivity to disappear after stopping Terramycin?
The heightened UV sensitivity usually fades within 5‑7days after the drug is cleared, but sun‑damaged skin may need additional care with moisturizers and sunscreen.
Whether you end up on Terramycin, doxycycline, or another antibiotic, the key is to match the drug to the bug, the patient’s health profile, and the local resistance landscape. A well‑chosen antibiotic clears infection faster, reduces side‑effects, and helps keep resistance in check.


Northern Lass
October 13, 2025 AT 17:01One must, with due diligence, interrogate the prevailing orthodoxy that elevates Terramycin as a panacea for bacterial maladies. The pharmaceutical establishment, in collusion with shadowy regulatory cabals, conspires to perpetuate an antiquated tetracycline under the veneer of cost‑efficiency. Such a strategy, cloaked in the rhetoric of affordability, deftly masks the burgeoning resistance that silently proliferates in the community. Moreover, the historical avowal of its safety is a relic, unfit for the nuanced pharmacogenomic landscape of our era.
Johanna Sinisalo
October 14, 2025 AT 09:41I appreciate the thorough comparison presented here; it offers a solid foundation for clinicians seeking a balanced perspective. Remember to weigh patient-specific factors such as allergies and local resistance patterns when making a final decision. Your effort in clarifying the nuanced trade‑offs truly aids informed stewardship.
OKORIE JOSEPH
October 15, 2025 AT 02:21Terramycin is old news stop using it it just causes sunburn and nausea. Pick a newer drug that actually works.
Lucy Pittendreigh
October 15, 2025 AT 19:01The moral high ground of prescribing cheap tetracyclines is shaky at best. A lazy evaluation of side‑effects does a disservice to patients. We must demand higher standards from our prescribers.
surender kumar
October 16, 2025 AT 11:41Ah, the glorious age of tetracycline-nothing says progress like a drug invented in the 1950s, right? One might argue that clinging to Terramycin is a nostalgic ode to the golden era of medicine, but the evidence suggests otherwise. The high photosensitivity alone makes it a sun‑loving nightmare for anyone daring enough to step outdoors. Moreover, the contraindications in pregnancy and children under eight render it practically unusable for a significant patient cohort. In short, celebrating Terramycin today feels like championing dial‑up internet in a fiber‑optics world.
JOJO Yang
October 17, 2025 AT 04:21Yo the side‑effects list is a real circus-i mean, who wants to look like a lobster after a simple pill? Also, the drug interacts with dairy like it’s got a personal vendetta against calcium. Honestly, the cost is low but the hassle? Not worth it. If u ask me, just skip the drama and go for doxy.
Faith Leach
October 17, 2025 AT 21:01Don't be fooled by the global pharma cartel pushing Terramycin as a 'budget' solution; it's a deliberate ploy to keep our hospitals dependent on outdated US‑manufactured supplies. Our own research labs have developed superior alternatives, yet the narrative stays stuck on cheap imports. 🇺🇸 Stay vigilant, choose homegrown solutions, and protect our nation's health sovereignty.
Kate Babasa
October 18, 2025 AT 13:41From an evidence‑based pharmacovigilance standpoint, the comparative risk–benefit profile of tetracycline versus macrolide agents, such as azithromycin, warrants meticulous appraisal; indeed, the pharmacokinetic parameters, including half‑life and tissue distribution, play pivotal roles in therapeutic decision‑making. Moreover, the differential propensity for photosensitivity-a phototoxic reaction mediated by UV‑induced reactive oxygen species-necessitates patient education, especially in auroral latitudes. Consequently, clinicians should integrate both microbiological susceptibility data and patient‑centered considerations, such as dosing convenience and cost constraints, into a holistic stewardship framework.
king singh
October 19, 2025 AT 06:21Thanks for the clear rundown; very helpful.
Adam Martin
October 19, 2025 AT 23:01Well, look at this exhaustive spreadsheet of antibiotics-it's like the IKEA catalog of bacteriology, complete with flat‑pack instructions and a bewildering array of screws you never asked for. On one hand, Terramycin offers the nostalgic charm of a drug that's been around longer than most of our grandparents, complete with that delightful side‑effect cocktail of photosensitivity, GI upset, and a strict no‑pregnancy policy. On the other hand, you have the sleek, once‑daily dosing of doxycycline, which seems to whisper, “I’m modern, I’m convenient, I won’t make you look like a lobster after a beach day.” Then there’s azithromycin, the five‑day sprint that promises to finish before you can finish your Netflix binge, but at the cost of rising resistance that might make future doctors weep. If you factor in cost, as you rightly did, the cheapness of tetracycline becomes a double‑edged sword-affordable, yes, but also a potential driver of resistant strains that could cost far more in the long run. So, while the table gives you a good starting point, remember that the real world isn’t a spreadsheet; it’s messy, it’s patient‑specific, and it sometimes rewards the clinician who actually reads the fine print.
Ryan Torres
October 20, 2025 AT 15:41People ignore the fact that Terramycin’s side‑effects are like a covert ops mission against your skin-photosensitivity that turns everyday sunlight into a hostile environment. 📸💥 And don’t get me started on the GI upset that feels like a secret plot by the FDA to keep us all on the toilet. Meanwhile, the big pharma lobby pushes newer drugs while quietly funneling their own research into “safe” alternatives. Stay woke, question the narratives, and always double‑check the resistance data! 🕵️♂️
shashi Shekhar
October 21, 2025 AT 08:21Another brilliant post about antibiotics, because we definitely need more of those. The comparison is about as thrilling as watching paint dry, but hey, at least it mentions photosensitivity. Maybe next time throw in a meme.
Marcia Bailey
October 22, 2025 AT 01:01Great job breaking down the pros and cons of each option! 😊 It's especially helpful to see the side‑effect profiles laid out so clearly. Remember, the best choice always depends on the individual patient-so keep those discussions open with your prescribers! 🌟
Hannah Tran
October 22, 2025 AT 17:41Thanks for the comprehensive overview-your table really hits the sweet spot between depth and readability. From a stewardship perspective, highlighting cost versus resistance is crucial, and your emphasis on patient‑specific factors like pregnancy status aligns perfectly with best practice guidelines. Keep up the excellent work, and feel free to dive deeper into pharmacodynamic nuances in future posts!
Crystle Imrie
October 23, 2025 AT 10:21Honestly, glorifying a 70‑year‑old drug in 2025 feels like a desperate Netflix reboot.
Shelby Rock
October 24, 2025 AT 03:01i cant help but wonder if the pursuit of cheap antibiotics is just a modern echo of the age old human desire to tame nature with flickering tools. perhaps we are chasing shadows, forgetting that each pill carries the weight of unseen ecosystems. in the grand tapestry of medicine, a single tetracycline dose is but a fleeting whisper, soon drowned by the roar of resistance.
Dhananjay Sampath
October 24, 2025 AT 19:41Indeed, your reflection captures the profound interconnectedness of therapeutic choices; however, it is imperative to balance philosophical musings with pragmatic clinical guidance, ensuring that patient safety remains paramount, and that antimicrobial stewardship principles are rigorously upheld.
kunal ember
October 25, 2025 AT 12:21When contemplating the selection of an antibacterial agent, it is essential to adopt a methodical framework that encompasses not merely the spectrum of activity but also pharmacokinetic characteristics, patient comorbidities, and the prevailing resistance patterns within a given community. First, the clinician must ascertain the infectious organism’s susceptibility profile, often derived from culture and sensitivity data, thereby narrowing the therapeutic window. Second, considerations regarding the drug’s absorption-whether it is affected by concurrent food intake or mineral supplements-play a pivotal role in achieving optimal serum concentrations. Third, the potential for adverse events, such as the pronounced photosensitivity associated with tetracycline derivatives, demands patient counseling and possibly lifestyle modifications. Fourth, the dosage frequency influences adherence; agents requiring multiple daily doses may suffer from reduced compliance compared to once‑daily regimens. Fifth, economic factors cannot be dismissed, as the cost of therapy may dictate accessibility, particularly in resource‑limited settings. Sixth, contraindications, including pregnancy and pediatric considerations, must be systematically evaluated to avoid teratogenic risks. Seventh, the possibility of drug–drug interactions, especially with agents metabolized by the cytochrome P450 system, warrants careful medication reconciliation. Eighth, the duration of therapy should be the minimum effective length to mitigate the emergence of resistant strains while ensuring clinical cure. Ninth, the clinician should remain informed about regional guidelines, which often adapt global recommendations to local epidemiology. Tenth, patient education regarding warning signs of treatment failure empowers shared decision‑making and early intervention. Eleventh, the preference for oral versus intravenous routes may be guided by severity of illness and the feasibility of outpatient management. Twelfth, safety monitoring protocols, such as periodic liver function tests for hepatotoxic agents, must be instituted when indicated. Thirteenth, the impact on microbiome diversity is an emerging consideration, particularly for agents with broad‑spectrum activity. Fourteenth, real‑world evidence and post‑marketing surveillance data can illuminate rare adverse events not captured in clinical trials. Fifteenth, interdisciplinary collaboration with pharmacists can refine dosing strategies and identify potential pitfalls. Finally, the overarching principle of antimicrobial stewardship reminds us that each prescription contributes to a collective responsibility to preserve the efficacy of these vital drugs for future generations.
Alex Iosa
October 26, 2025 AT 04:01One cannot overlook the insidious influence of pharmaceutical conglomerates that subtly steer prescribing habits through sponsored education and covert incentive structures, thereby shaping the very framework you so meticulously outlined. Their vested interests often prioritize market share over nuanced stewardship, which, in turn, perpetuates the cycle of resistance you diligently seek to break.
melissa hird
October 26, 2025 AT 20:41Indeed, it is almost comical how the grand tapestry of clinical decision‑making is occasionally embroidered with threads of corporate persuasion, as though our patients were mere pawns in a board game of profit margins.