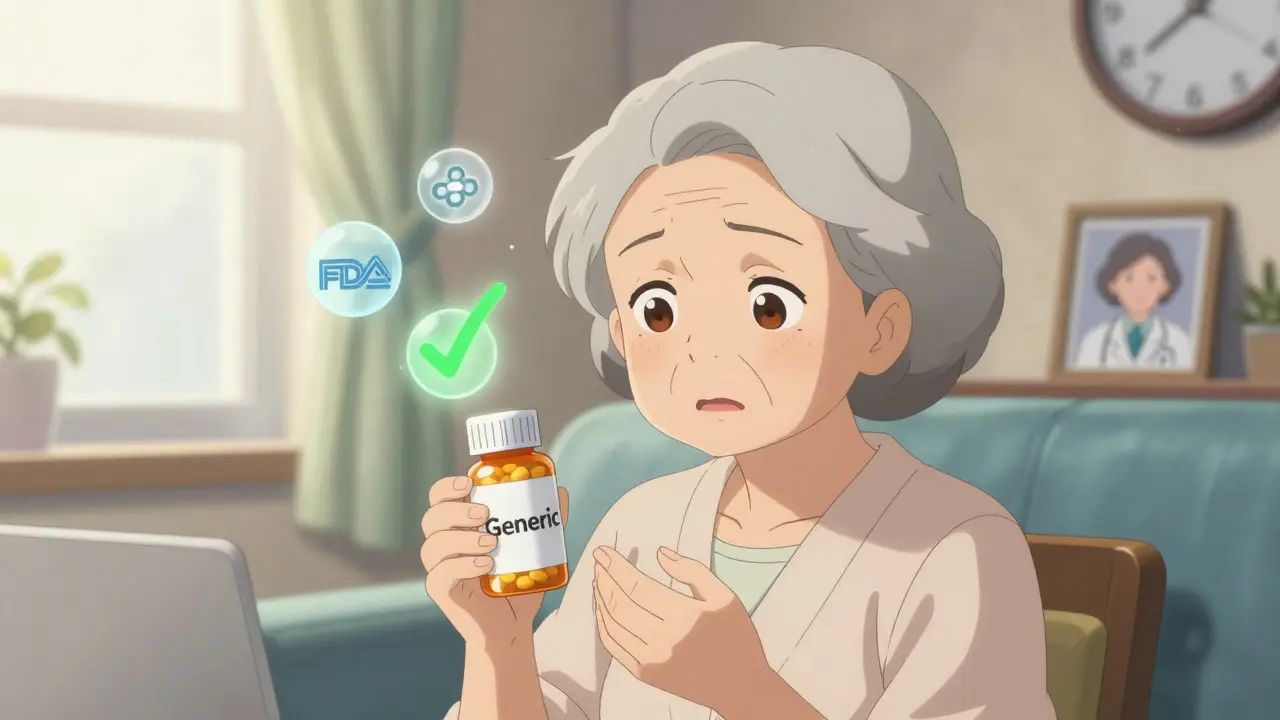
When you walk into a pharmacy and your doctor prescribes a medication, you expect the pill you get to work the way it should. But what if the pill you’re handed is labeled as a generic version? For many patients, that label triggers a quiet doubt: Is this really the same?
The science says yes. The U.S. Food and Drug Administration (FDA) requires generic drugs to match brand-name drugs in strength, dosage, safety, and how fast they work. They must deliver the same active ingredient within a narrow range - 80% to 125% of the brand’s absorption rate. That’s not a guess. It’s a strict, tested standard. Yet, despite decades of data and millions of prescriptions filled, nearly one in five patients still believe generic drugs are less safe.
Why Do Patients Doubt What the Science Proves?
It’s not about ignorance. It’s about perception. The word "generic" itself carries baggage. In everyday life, "generic" means basic, plain, maybe even cheap. Think generic cereal versus Kellogg’s. Generic phone cases versus Apple. People don’t assume the generic version is worse - they just assume it’s different. And when it comes to your health, "different" feels risky.
Studies show that patients often link price to quality. If a brand-name drug costs $100 and the generic costs $5, it’s hard not to wonder: Why is it so much cheaper? What’s missing? That’s not logic - it’s psychology. Dr. Aaron S. Kesselheim from Harvard found that simply calling a drug "generic" triggers a mental shortcut: lower cost = lower quality. Even when patients know the facts, that gut feeling lingers.
The Real Triggers: Personal Experience Over Data
Numbers don’t convince people. Stories do.
Take John, a 68-year-old from Ohio. His doctor switched his blood pressure medication from the brand-name version to a generic. A few weeks later, his numbers went up. He went back to the brand. His numbers stabilized. He told his friends: "The generic didn’t work for me. I won’t take it again."
John’s experience isn’t rare. On Reddit, forums like r/pharmacy are full of similar stories - patients who switched to generic sertraline, bupropion, or levothyroxine and felt worse. Some reported withdrawal symptoms, fatigue, or mood swings. When they switched back, things improved.
Here’s the twist: the FDA has found no consistent pattern of failure in these cases. In fact, 68% of patients who switch to generics report no difference at all. But those 32% who do notice a change? Their stories become louder than the data. And that’s how myths grow.
Even more troubling: some generic versions have had issues. In 2012, the FDA issued a safety notice about certain generic bupropion XL tablets. A small number of patients reported reduced effectiveness. That wasn’t a failure of all generics - it was a failure of one manufacturer’s formulation. But the damage was done. The headline wasn’t "One generic product recalled." It was "Generic antidepressants may not work." And that stuck.
Who’s Most Likely to Fear Generics?
It’s not random. Certain groups are far more likely to avoid generics - and the reasons are tied to life experience, not just education.
- Patients over 60 are 31.9% more likely to worry about side effects than younger users.
- Those with less education are nearly twice as likely to believe generics are dangerous.
- Black and Hispanic patients are 1.8 times more likely to express safety concerns than White patients.
- Unemployed and retired patients are more open to generics - likely because cost matters more than perceived risk.
- Rural patients often believe generics are "weaker" and need higher doses - a myth with no scientific basis.
And here’s the kicker: patients cared for by specialists are 27% less likely to be prescribed generics than those seeing primary care doctors. Why? Specialists often work in settings where brand-name drugs are more familiar. They’re less likely to have the time or training to explain bioequivalence. So the message patients get isn’t "This is safe" - it’s "This is what we’ve always used."

Doctors and Pharmacists: The Missing Link
The biggest predictor of whether a patient accepts a generic? How their provider talks about it.
Dr. William Shrank’s research found that patients who received a simple explanation - "This generic has the same active ingredient and works the same way" - were 3.2 times more likely to agree to the switch. That’s not a small boost. That’s a game-changer.
Yet most providers don’t say anything. In a 2018 study, the average time a pharmacist spent explaining a generic substitution was 47 seconds. That’s less than a tweet. No wonder patients leave confused.
But when pharmacists take the time - even just two minutes - to say, "I’ve filled this for hundreds of patients. No one’s reported problems. The FDA checks these batches every month," adherence jumps by 37%. That’s the power of a trusted voice.
What About the Quality of the Pills?
One of the biggest fears? "Are generics made in sketchy factories?"
The truth: over 70% of generic drugs sold in the U.S. are made in facilities that are inspected by the FDA - same as brand-name drugs. Many are made in the same factories. The difference? The brand-name company sells the drug under its name. The generic company sells it under the chemical name. The pill? Identical.
The FDA has spent over $150 million since 2012 to improve oversight of generic manufacturing. They inspect plants in India, China, and the U.S. with the same standards. But most patients don’t know that. And when you hear stories about "foreign-made pills," it’s easy to imagine shady labs. The reality? Most facilities follow strict protocols. But perception doesn’t care about facts.
The Economic Cost of Doubt
Here’s what’s at stake: generics make up 90% of all prescriptions filled in the U.S. But they account for only 23% of drug spending. That’s because people keep asking for the brand-name version - even when the generic is cheaper and just as effective.
The Congressional Budget Office estimates that if everyone accepted generics, the U.S. could save $185 billion over the next decade. Right now, brand loyalty costs the system $8 billion a year in unnecessary prescriptions.
Insurance plans that offer $0 copays for generics see 18% higher use. Why? Because when cost isn’t a barrier, people are more willing to try. But even then, some still refuse - because they don’t trust it.
What’s Changing? And What’s Not
The FDA launched a new education campaign in 2023, targeting Spanish-speaking communities with videos, brochures, and social media. Preliminary results show a 15% drop in safety concerns among those groups. That’s progress.
But new challenges are rising. Complex generics - like inhalers, eye drops, and topical creams - are harder to prove equivalent. Patients notice. A 2023 survey found 48% of patients specifically worry about these types of drugs. They’re right to be cautious - because bioequivalence is harder to measure. But that doesn’t mean they’re unsafe. It just means the science is more complex.
And then there’s the "authorized generic" loophole. Sometimes, the brand-name company sells its own drug under a generic label. It’s the exact same pill - same factory, same formula. But patients see it as "brand-name in disguise." And that makes them more suspicious. "If it’s the same, why did they make a generic version?"
How to Overcome the Fear
Here’s what works - backed by real data:
- Explain at the point of prescribing. Don’t wait until the pharmacy. Say it when you write the script: "This generic is approved by the FDA and works exactly like the brand."
- Use plain language. Avoid terms like "bioequivalence." Say: "Same medicine. Same effect. Just cheaper."
- Let pharmacists talk. Give them time. Even 90 seconds makes a difference.
- Target high-risk groups. Older adults, lower-income patients, non-English speakers - they need tailored messages.
- Share success stories. "Over 100,000 people switched to this generic. Most saw no change."
It’s not about convincing everyone. It’s about reducing the fear that stops people from taking the medicine they need.
Final Thought
Patients aren’t irrational. They’re responding to signals - a cheaper price, a different-looking pill, a doctor who never explained the switch, a friend who had a bad experience.
The science is clear: generics are safe. But trust isn’t built with data. It’s built with time, clarity, and human connection. Until providers start treating perception as part of treatment, the gap between what’s true and what’s believed will stay wide. And the cost? Not just money. It’s health.
Are generic drugs really as safe as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict manufacturing standards. Studies show they work the same way in the body - within a 80% to 125% range of absorption. Millions of patients use generics safely every day.
Why do some people feel worse after switching to a generic?
Some patients report side effects or reduced effectiveness after switching, but this is rare and often not due to the drug itself. It can be caused by changes in inactive ingredients (like fillers), which may affect how the body absorbs the medicine slightly. In rare cases, a specific generic formulation had issues - like certain bupropion XL tablets in 2012. But these are exceptions, not the rule. Most patients experience no difference at all.
Do generics come from unsafe factories?
No. Over 70% of generic drugs sold in the U.S. are made in FDA-inspected facilities - the same ones that make brand-name drugs. The FDA inspects plants in the U.S., India, China, and elsewhere using the same standards. Many generics are made in the exact same factories as brand-name versions. The difference is only in the label.
Why do doctors sometimes avoid prescribing generics?
Some doctors don’t prescribe generics because they’re unfamiliar with the options, lack time to explain them, or assume patients prefer brand-name drugs. Specialists are less likely to prescribe generics than primary care doctors. It’s not because generics are unsafe - it’s often because communication gaps exist between providers and patients.
Can I trust generics for serious conditions like heart disease or epilepsy?
Yes. The FDA approves generics for all conditions, including life-threatening ones. Studies have shown no difference in outcomes for patients using generic versions of heart medications, epilepsy drugs, and blood thinners. In fact, most hospitals use generics for these drugs because they’re proven safe and cost-effective. Fear often comes from stories - not science.

Andy Cortez
February 7, 2026 AT 10:58Joseph Charles Colin
February 8, 2026 AT 03:58Randy Harkins
February 9, 2026 AT 05:41Tori Thenazi
February 9, 2026 AT 17:42Frank Baumann
February 11, 2026 AT 16:09Alex Ogle
February 13, 2026 AT 06:17Brandon Osborne
February 14, 2026 AT 15:03Lyle Whyatt
February 15, 2026 AT 03:06Random Guy
February 16, 2026 AT 14:24Chelsea Cook
February 16, 2026 AT 15:24John Sonnenberg
February 17, 2026 AT 16:21Jessica Klaar
February 17, 2026 AT 17:37