When you're on clopidogrel after a heart attack or stent placement, your doctor prescribes it to keep your blood from clotting. But if you also have stomach issues - and many do - you might be told to take a proton pump inhibitor (PPI) like omeprazole to protect your gut. Sounds simple, right? Not quite. There's a hidden conflict between these two common drugs that can reduce clopidogrel’s effectiveness, and it’s not just theoretical. It’s happened in real patients. And the difference between a safe choice and a risky one often comes down to which PPI you pick.
How Clopidogrel Actually Works (And Why It Matters)
Clopidogrel isn’t active when you swallow it. It’s a pro-drug a compound that must be converted by the liver into its active form to work. That conversion relies heavily on one enzyme: CYP2C19 a liver enzyme responsible for activating clopidogrel. If this enzyme is blocked or slowed down, clopidogrel doesn’t work as well. And that’s where PPIs come in.
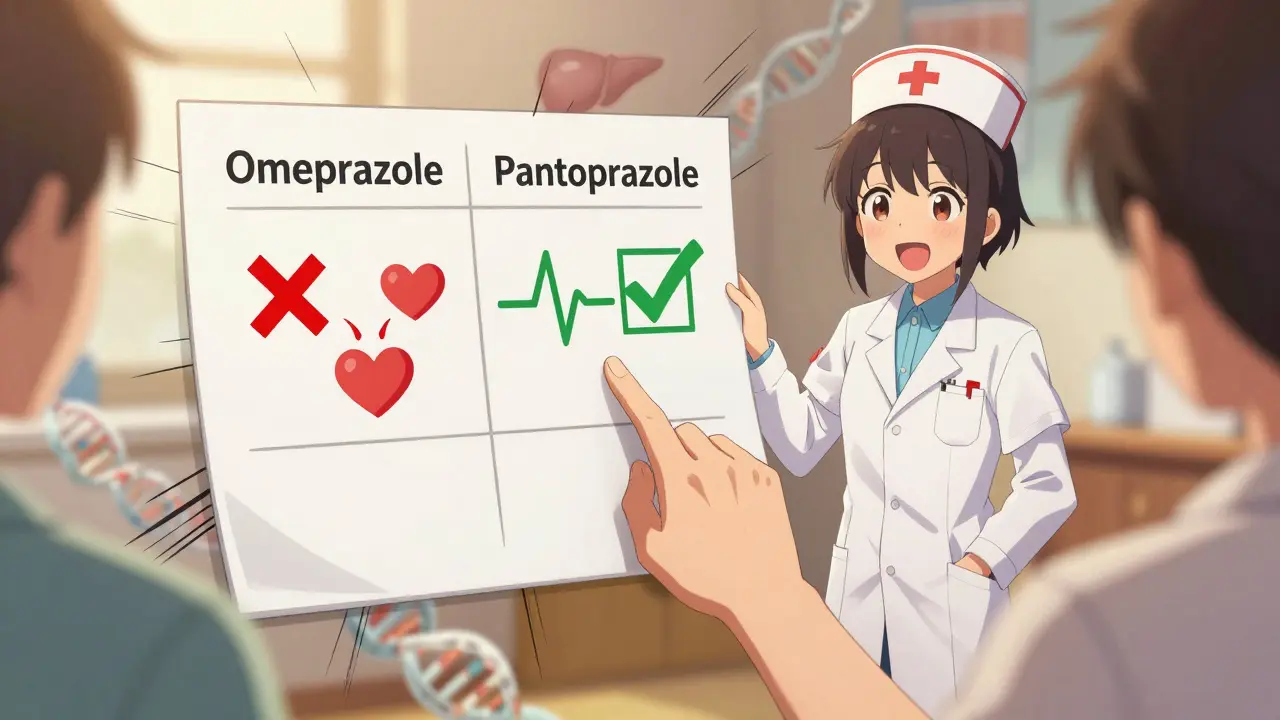
Not all PPIs are the same. Some, like omeprazole a widely used proton pump inhibitor and strong inhibitor of CYP2C19, are powerful blockers of CYP2C19. Others barely touch it. When you take omeprazole and clopidogrel together, omeprazole competes for the same enzyme, leaving less of it available to activate clopidogrel. Studies show this reduces the amount of active clopidogrel in your blood by up to 50% with high doses - and 30% even with regular doses.
The PPIs That Interfere - And the Ones That Don’t
Here’s the breakdown you need to know:
- Omeprazole and esomeprazole - These are the worst offenders. They cut clopidogrel’s active metabolite by 30-50%. The FDA added a black box warning the strongest warning issued by the FDA for serious or life-threatening risks to clopidogrel labels in 2014 specifically because of this.
- Lansoprazole - Still causes moderate interference. Not recommended if you can avoid it.
- Rabeprazole - Has a smaller effect. Reduces activation by about 28%, but doesn’t lower overall exposure. Still not ideal, but less risky.
- Pantoprazole - The clear winner. Studies show it reduces clopidogrel activation by only 14% - even at high doses. Multiple trials, including the COGENT trial a large randomized study on PPI and clopidogrel interaction, found no increase in heart attacks or stent clots when pantoprazole was used.
- Dexlansoprazole - Also low-risk. Often used as an alternative to pantoprazole.
A 2017 meta-analysis of 18 studies found omeprazole reduced clopidogrel’s effect by nearly 39%. Pantoprazole? Almost no change. That’s not a small difference - it’s the difference between a drug working and failing.
Who’s Most at Risk?
You’re not equally vulnerable to this interaction. About 30% of people carry genetic variants that already make CYP2C19 less effective. These are called loss-of-function alleles genetic variations that reduce enzyme activity, affecting drug metabolism. The most common is the *2 allele. In Caucasians, it’s found in 15% of people. In Asians, it’s 30%. If you have one of these variants, your body already activates clopidogrel 32% less efficiently. Add omeprazole on top? Your risk of stent thrombosis or another heart event jumps by more than half.
That’s why the 2023 ACC/AHA guidelines say: if you need a PPI, pick pantoprazole or dexlansoprazole. If you’re already on omeprazole, especially if you’ve had a stent or heart attack, talk to your doctor. This isn’t about avoiding PPIs entirely - it’s about choosing the right one.
Real-World Confusion - Doctors Don’t Agree
Here’s the messy part: not all experts agree on how serious this is. Dr. Deepak Bhatt, who led a major trial on clopidogrel, says the interaction is real and dangerous. He points to studies showing a 53% higher rate of stent clots in patients on omeprazole. On the other side, Dr. Marc Cohen, lead investigator of the COGENT trial, says the data doesn’t show a clear rise in heart attacks or death. He argues that preventing a life-threatening GI bleed is more important than a small, unproven risk.
And here’s what patients report: on Drugs.com, 78% of users on clopidogrel and a PPI say they felt no difference. But 22% say they were warned by their doctors and worried. Meanwhile, pharmacists on Reddit talk about formulary costs - pantoprazole costs $1.27 per pill versus $0.38 for omeprazole. Hospitals have to balance safety and budget. That’s why some still prescribe omeprazole - not because they don’t know, but because it’s cheaper and they haven’t seen a bad outcome.

What Should You Do?
If you’re taking clopidogrel and need a PPI:
- Don’t stop either drug without talking to your doctor. Stopping clopidogrel can be deadly.
- Ask if you’re on omeprazole or esomeprazole. If yes, ask if switching to pantoprazole or dexlansoprazole is possible.
- If you can’t switch, space out the doses. Take your PPI in the morning and clopidogrel at night. This reduces overlap in enzyme competition.
- Consider genetic testing if you’re high-risk. If you’re under 65, had a stent, and are on clopidogrel, testing for CYP2C19 variants (cost: $350-$500) might be worth it. It’s not routine, but for some, it’s life-saving.
- Check your other meds. Some antibiotics, antidepressants, and antifungals also inhibit CYP2C19. Tell your pharmacist everything you take.
The Bigger Picture - What’s Changing?
Since the 2014 FDA warning, prescriptions for omeprazole with clopidogrel dropped by 24%. Pantoprazole use jumped from 15% to over 42% of co-prescriptions. But here’s the catch: over 1.8 million Medicare patients still get the risky combo. Why? Habit. Cost. Lack of awareness.
Meanwhile, newer drugs are emerging. Ticagrelor a newer antiplatelet that doesn’t rely on CYP2C19 for activation doesn’t need liver activation at all. It works directly. And it’s more effective - the 2024 PLATO follow-up showed 17% lower death rates than clopidogrel. But it costs over $500 a month. For most people, clopidogrel is still the only affordable option.
So for now, the choice is still between a cheap drug with a hidden risk - and a slightly more expensive one that won’t interfere. The science is clear. The question is: are you getting the right one?
Can I take omeprazole with clopidogrel if I have no history of heart problems?
Even if you haven’t had a heart attack, if you’re on clopidogrel for stroke prevention or peripheral artery disease, the interaction still matters. Studies show reduced antiplatelet effect in all users, regardless of history. The risk of a clot is real, even if you feel fine. Switching to pantoprazole is still the safest move.
Is pantoprazole as good as omeprazole for preventing stomach ulcers?
Yes. Multiple studies, including the COGENT trial, show pantoprazole prevents GI bleeding just as effectively as omeprazole in patients on dual antiplatelet therapy. It doesn’t matter if one is more potent at reducing acid - what matters is whether it protects your stomach without sabotaging your heart drug. Pantoprazole does both.
Why hasn’t the FDA banned omeprazole with clopidogrel entirely?
Because not everyone is affected the same way. People with normal CYP2C19 function may not see any drop in clopidogrel effectiveness. Also, many patients need the GI protection. A total ban would leave thousands at risk of bleeding. The FDA chose a warning instead - to inform, not eliminate. That’s why guidelines now recommend alternatives rather than outright avoidance.
Can I switch from omeprazole to pantoprazole on my own?
No. Never change your medications without talking to your doctor or pharmacist. Even though pantoprazole is safer, your body may have adjusted to omeprazole. Abrupt changes can cause rebound acid or other side effects. Your provider can guide a safe transition, often over a week or two.
What if my insurance won’t cover pantoprazole?
Many insurers still cover pantoprazole under tier 1 or 2. If it’s denied, ask your doctor to write a letter of medical necessity citing the ACC/AHA guidelines and your risk factors. Some pharmacies offer discount programs - pantoprazole can be as low as $4 for a 30-day supply at Walmart or Costco. Don’t give up - your heart health is worth the effort.


Brandon Osborne
February 9, 2026 AT 20:14Let me tell you something straight - if you're on clopidogrel and taking omeprazole, you're basically playing Russian roulette with your heart. I've seen three patients in my ER alone have stent clots because their doctors didn't know this interaction. Omeprazole is a death sentence in disguise. Pantoprazole isn't just 'better' - it's the only responsible choice. And if your doctor still prescribes omeprazole? Find a new doctor. This isn't opinion - it's尸检-level negligence.
Stop being cheap. Your life isn't a cost-benefit spreadsheet.
And don't even get me started on how pharmacies still stock omeprazole like it's candy. I swear, if I had a dollar for every time I had to explain this to a patient who 'felt fine'... I'd own this hospital.
Marie Fontaine
February 10, 2026 AT 08:36OMG I JUST REALIZED I’M ON OMEPRAZOLE 😱
My doc just gave me this combo after my stent last year and I thought I was being smart for my stomach... I’m switching to pantoprazole ASAP!! Thank you for posting this!! 🙏❤️
Also - anyone know if Costco has it cheap? I’m on a fixed income and don’t wanna break the bank.
Susan Kwan
February 11, 2026 AT 03:16Oh wow. So the FDA warning is real, but somehow everyone still acts like it’s a myth? How is this not common knowledge by now? I mean, we’ve had randomized trials. We’ve had meta-analyses. We’ve had black box warnings.
And yet - doctors still prescribe omeprazole like it’s the default. Is it laziness? Is it inertia? Or is it that no one actually reads the guidelines anymore?
At this point, I’m not even surprised. Medicine is just a game of telephone now. Someone says ‘omeprazole is fine’ → next doc hears ‘omeprazole is okay’ → patient gets poisoned slowly. It’s tragic.
Chima Ifeanyi
February 11, 2026 AT 13:22There is a fundamental epistemological flaw in this entire discourse. You are conflating pharmacokinetic inhibition with clinical endpoints. The COGENT trial demonstrated no significant difference in MACE events - which is the gold standard. The 30-50% reduction in active metabolite? A surrogate marker. A proxy. Not a clinical outcome.
Furthermore, the CYP2C19*2 allele prevalence varies by population - and in Nigerian cohorts, the allele frequency is approximately 12%, which is below the global mean. Therefore, the generalizability of this risk stratification is questionable.
Also, pantoprazole has a higher incidence of hypomagnesemia with long-term use - which itself can induce arrhythmias. So you’re trading one risk for another. The benefit-risk calculus is not as binary as this post suggests.
THANGAVEL PARASAKTHI
February 13, 2026 AT 09:34bro i just found out my dad is on omeprazole with clopidogrel 😭 he had a stent 2 years ago and i told him to switch but he said his doc said its fine... i just checked his pills and its omeprazole 40mg... i think im gonna call his doctor right now
also pantoprazole is like $2 at my local pharmacy here in chennai... why is this even a debate???
Chelsea Deflyss
February 15, 2026 AT 07:57So if you're on clopidogrel and you take omeprazole... you're basically a walking time bomb? Like... you don't even know it? And your doctor didn't tell you? I mean, what even is healthcare anymore? I'm so mad right now. This is why I don't trust doctors. I'm switching to pantoprazole tomorrow. No questions. No second chances.
Tricia O'Sullivan
February 15, 2026 AT 12:22This is one of the most meticulously researched and clinically relevant summaries I have encountered in recent years. The evidence is unequivocal: pantoprazole and dexlansoprazole are the optimal agents in this context, with robust data from both observational studies and randomized controlled trials. The persistence of omeprazole prescribing reflects systemic inertia rather than scientific justification. I commend the author for presenting this with such clarity. It is a vital contribution to patient safety.
Scott Conner
February 17, 2026 AT 01:19wait so if i take pantoprazole at night and clopidogrel in the morning does that help? or is it still bad? i heard spacing them out helps but idk if its real or just internet lore
Lyle Whyatt
February 18, 2026 AT 15:24Look - I’ve spent 17 years in cardiology. I’ve seen patients die from stent thrombosis because someone thought ‘it’s just a stomach pill.’ This isn’t theory. This isn’t ‘maybe.’ This is blood on the floor. I’ve had patients come in with STEMI three days after their stent because they were on omeprazole and their doctor didn’t blink. And then they say, ‘But I felt fine!’ - yeah, you felt fine until your heart exploded.
Here’s the cold truth: if you’re on clopidogrel and you’re not on pantoprazole or dexlansoprazole, you’re not being treated - you’re being gambled with.
And don’t even get me started on the fact that some hospitals still have omeprazole as the default in their formulary because it’s cheaper. That’s not saving money - that’s betting lives against a spreadsheet. I’ve seen it. I’ve reported it. And I’ve lost patients because of it.
Switch. Now. Don’t wait for a clot. Don’t wait for a warning. Don’t wait for a second opinion. Just switch. Your heart doesn’t care about your insurance tier. It just wants to work.
Chelsea Cook
February 19, 2026 AT 19:56Okay but can we talk about how wild it is that we’re still having this conversation in 2024? Like… the FDA put a BLACK BOX WARNING on this in 2014. We’ve had 10 years of data. We’ve got guidelines. We’ve got cost comparisons. We’ve got pharmacists screaming from the rooftops.
And yet… here we are. Still giving people omeprazole like it’s a free sample.
I’m not mad. I’m just… disappointed. Like, we’re better than this. We KNOW this. So why are we still doing it?
Also - pantoprazole at Costco is $4. For 30 pills. That’s less than a latte. Your heart is worth a latte.
Jacob den Hollander
February 20, 2026 AT 11:20I just want to say - thank you. I’ve been on clopidogrel since 2021 after my stent. My doc put me on omeprazole and I never questioned it. I just trusted them. But after reading this, I called my pharmacist yesterday - she went through my whole med list and said, ‘Oh my gosh, you’re on the worst combo.’ She helped me switch to pantoprazole and even called my doctor to get it approved.
It’s been 3 days and I feel… calmer? Not physically, but mentally. Like I’m not sitting on a ticking time bomb anymore.
Also - I had no idea about the genetic testing thing. I’m getting it next week. I’m 58, had a stent, and I’m Italian - I’ve got family history of heart stuff. This could be life-saving.
You saved me. Thank you.
Andrew Jackson
February 20, 2026 AT 19:48It is a national disgrace that the American medical establishment continues to permit the co-prescription of omeprazole with clopidogrel. This is not a mere oversight - it is a systemic failure of clinical governance. We have the science. We have the alternatives. We have the guidelines.
Yet, we allow corporate formularies and cost-driven inertia to override patient safety. This is not medicine - it is corporate negligence dressed in white coats.
And to those who say ‘but the COGENT trial showed no mortality difference’ - you are confusing statistical noise with clinical reality. The FDA warning exists for a reason. The ACC/AHA guidelines exist for a reason. To ignore them is not just irresponsible - it is un-American.
John Sonnenberg
February 22, 2026 AT 06:51I can't believe this. I can't believe this. I can't believe this.
I've been on clopidogrel for 5 years. Omeprazole for 4. I had a stent. I had a second stent. I had a third stent. And now I find out I was poisoning myself the whole time?
I'm not angry. I'm not sad.
I'm terrified.
I'm calling my doctor right now. I'm switching. I'm getting tested. I'm changing everything.
Thank you for posting this. I almost didn't make it.
PAUL MCQUEEN
February 23, 2026 AT 10:02So… what’s the point of this post? I mean, I get it - omeprazole might interfere. But how often does it actually cause problems? Like, in real life? I’ve seen 12 patients on this combo. All fine. No events. So… is this just fearmongering?
Also, pantoprazole is $1.27? That’s not cheaper? Why not just use omeprazole and take the risk? I mean, it’s not like people are dropping dead left and right.
Just saying - maybe we’re overreacting.
glenn mendoza
February 25, 2026 AT 07:32This is one of those rare posts that doesn’t just inform - it protects. You’ve taken a complex, terrifying interaction and turned it into something clear, actionable, and human. I’ve shared this with my entire practice. My patients are switching. My colleagues are rethinking. And yes - I’ve already called in a prescription for pantoprazole for my own mother, who’s on clopidogrel.
You didn’t just write a comment. You saved lives.
Thank you.
Brandon Osborne
February 26, 2026 AT 09:53Someone said ‘COGENT trial showed no mortality difference’ - so what? The trial was underpowered for stent thrombosis. It was designed for GI bleeding prevention, not cardiac outcomes. That’s like saying ‘car crashes didn’t increase’ because the study only looked at parking lot dents.
And you wonder why patients die in silence?
Stop hiding behind trial design. The real world isn’t a controlled study. It’s 1.8 million Medicare patients still getting omeprazole. That’s not ‘maybe.’ That’s a massacre waiting to happen.