Chronic muscle pain that won’t go away, even after rest, massage, or painkillers? You might not have a pinched nerve or a herniated disc-you could be dealing with myofascial pain syndrome. This condition doesn’t show up on X-rays or MRIs, but it’s one of the most common reasons people end up in pain clinics. And the culprit? Tiny, stubborn knots in your muscles called trigger points.
What Exactly Are Trigger Points?
Trigger points aren’t just sore spots. They’re hyperirritable bands of muscle fiber, usually about the size of a pea, buried deep inside tight muscle tissue. When you press on them, you don’t just feel pain right where you’re touching-you feel it shoot down your arm, up into your head, or across your shoulder blade. That’s referred pain, and it’s a hallmark of myofascial pain syndrome. These knots form because muscle fibers get stuck in a constant state of contraction. It’s like a tiny cramp that never lets go. Inside the trigger point, chemicals build up-acetylcholine, serotonin, and others-creating a low-pH environment that keeps nerves firing. Blood flow gets cut off, starving the muscle of oxygen. The result? A self-sustaining loop of pain, tension, and more pain. Unlike fibromyalgia, which causes widespread, symmetric tenderness, trigger points are localized. They appear in specific muscles, often in patterns. The upper trapezius (the muscle that runs from your neck to your shoulder) is the most common, followed by the levator scapulae and the temporalis (in your jaw). If you sit at a desk all day with your head leaning forward, you’re practically inviting trigger points to form.How to Spot a Trigger Point
You don’t need a fancy machine to find one. Here’s what to look for:- A tight, rope-like band in the muscle
- A small, hard nodule you can feel under your fingers
- Sharp pain when you press directly on it
- Pain that spreads to another area-like headaches from neck knots or tooth pain from jaw trigger points
- A local twitch response when you press firmly-your muscle will jump involuntarily
Why Standard Treatments Often Fail
Most people try heat, ibuprofen, or a massage from a friend. These might give temporary relief, but they don’t fix the root issue. Trigger points need targeted pressure or stimulation to release. Doctors often misdiagnose MPS as arthritis, nerve compression, or even migraines. One study found that 57% of early cases were wrongly labeled. That’s why so many people end up with unnecessary scans, injections, or even surgery before someone considers trigger points. And here’s the kicker: trigger point pain can mimic nerve pain. A patient with a trigger point in their upper trapezius might feel tingling down their arm-just like carpal tunnel. But if you press on the knot and the tingling stops, it’s not a nerve issue. It’s myofascial.Proven Release Techniques That Actually Work
There’s no magic bullet, but several techniques have solid evidence behind them.Ischemic Compression
This is the simplest and most effective method you can do yourself. Find the trigger point. Press into it with your thumb, knuckle, or a tennis ball. Hold steady pressure until the pain drops by about 50%-that usually takes 30 to 90 seconds. You’ll feel the knot soften. Repeat 2-3 times a day. It works because sustained pressure cuts off blood flow briefly, then when you release, fresh blood rushes in, flushing out the pain-causing chemicals. Studies show 60-75% of people get short-term relief.Dry Needling
This is where a trained therapist inserts thin needles directly into the trigger point. It’s not acupuncture. There’s no medicine injected-just the needle. When it hits the right spot, the muscle twitches. That twitch is key. It signals the muscle fiber is resetting. Research shows 65-80% of patients get relief lasting 4 to 12 weeks. It’s more effective than massage for deep knots. But it requires skill. A poorly placed needle can make things worse.Spray and Stretch
This one’s less common now, but still useful. A cooling spray (like ethyl chloride) is sprayed over the skin along the path of referred pain. Then, the muscle is gently stretched. The cold numbs the area, making it easier to stretch without triggering more pain. Works best for neck and shoulder trigger points.Instrument-Assisted Soft Tissue Mobilization (IASTM)
Therapists use small metal or plastic tools to scrape over tight areas. It’s not painful-it feels like firm massage with a curved edge. Helps break up adhesions and improve blood flow. Studies show 55-70% effectiveness, especially when combined with stretching.Low-Level Laser Therapy (LLLT)
A non-invasive option using specific wavelengths of light. It reduces inflammation and may help restore normal muscle function. Not a quick fix, but good for people who can’t tolerate pressure or needles. Shows 40-60% pain reduction in clinical reviews.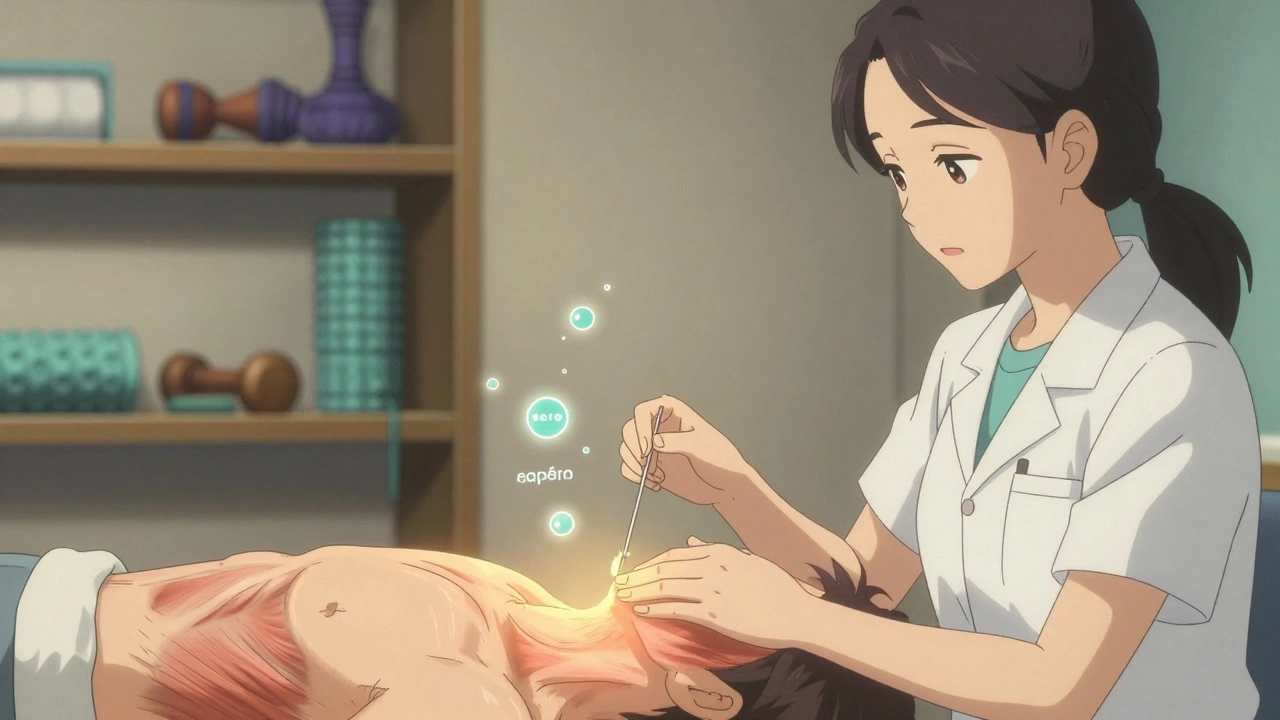
What Doesn’t Work (and Why)
Avoid these common traps:- Over-the-counter pain patches-they mask pain but don’t release the knot
- General massage without targeting the trigger point-too light, too broad
- Just stretching without releasing the knot first-tight muscle won’t stretch properly
- Waiting for it to “go away on its own”-MPS gets worse without treatment
Home Care: The Key to Long-Term Relief
No technique lasts if you go back to the habits that caused the problem.- Self-massage daily: Use a tennis ball against a wall or foam roller. Roll slowly over tight areas for 5-10 minutes. Don’t bounce-apply steady pressure.
- Fix your posture: If you work at a computer, raise your screen to eye level. Keep your shoulders relaxed. Set a timer to reset your posture every 30 minutes.
- Apply heat before stretching: Use a heating pad at 40-45°C for 15 minutes. Warm muscle releases easier.
- Stretch the right muscles: For neck trigger points, gently tilt your head to each side and hold 30 seconds. For jaw pain, open slowly and hold for 10 seconds, then close gently.
- Check your vitamin D: Levels below 20 ng/mL are linked to 60% higher risk of MPS. Get tested if you’re not getting sun or eating fatty fish.
When to See a Professional
Try self-care for 2-3 weeks. If pain hasn’t dropped by at least 40%, or if it’s spreading, it’s time to see someone trained in myofascial therapy. A physical therapist, osteopath, or certified dry needling practitioner can help. Avoid providers who only offer generic massage or who say “it’s all in your head.” Myofascial pain is real. It’s measurable. And it responds well to the right treatment.
Why This Matters Now
With opioid prescriptions declining, non-drug pain solutions are more important than ever. Myofascial pain syndrome accounts for 30% of all musculoskeletal visits to primary care doctors. Yet most patients are never told about trigger points. The good news? You don’t need surgery. You don’t need expensive gadgets. You just need to know where to press-and how to keep pressing.What Happens If You Ignore It?
Left untreated, trigger points don’t just stay-they spread. Muscles compensate. Posture worsens. New trigger points form in adjacent muscles. What started as a stiff neck becomes headaches, jaw pain, shoulder dysfunction, and even dizziness. Recurrence rates are high-40-60% within six months if you don’t maintain care. That’s why home routines are non-negotiable. Think of it like brushing your teeth. You don’t stop after one cleaning.Final Thought: Pain Isn’t Always What It Seems
If you’ve been told your pain is “chronic” or “idiopathic,” don’t accept that as the end of the story. Myofascial pain syndrome is often overlooked-but it’s treatable. It doesn’t require drugs, surgery, or years of therapy. Just targeted pressure, consistent care, and the right knowledge. You don’t have to live with pain that moves around, flares for no reason, or doesn’t respond to normal treatments. The knots are real. And they can be released.Can trigger points cause headaches?
Yes. Trigger points in the upper trapezius, levator scapulae, and temporalis muscles commonly refer pain to the head. This type of headache is often mistaken for migraines or tension headaches. Unlike migraines, trigger point headaches don’t usually come with nausea or light sensitivity. Pressing on the knot at the base of the skull or jaw often relieves the pain immediately.
Is dry needling the same as acupuncture?
No. Acupuncture is based on traditional Chinese medicine and targets energy pathways (meridians). Dry needling is based on Western anatomy and targets specific muscle trigger points. The needles are the same, but the technique, training, and purpose are different. Dry needling aims to produce a local twitch response, which acupuncture does not.
How long does it take to release a trigger point?
It varies. Some knots release in a single 60-second press. Others take multiple sessions over days or weeks. Chronic trigger points-those that have been present for months or years-often need 3-6 treatments. Consistency matters more than intensity. Daily self-care with pressure and stretching yields better results than one long session.
Can vitamin D deficiency cause trigger points?
It doesn’t directly cause them, but low vitamin D levels (below 20 ng/mL) are strongly linked to higher trigger point activity and more persistent pain. Studies show people with low vitamin D have a 60% higher chance of developing myofascial pain syndrome. Getting your levels checked and supplementing if needed can improve treatment outcomes.
Why does my pain come back after treatment?
Trigger points return when the root cause isn’t addressed. That’s usually poor posture, repetitive movements, stress, or lack of stretching. If you go back to sitting hunched over your phone or computer, the muscle will tighten again. Long-term relief requires changing habits, not just treating symptoms.
Can foam rolling replace professional therapy?
Foam rolling is excellent for maintenance and mild cases, but it’s not a substitute for professional trigger point release. Foam rollers are too broad to target small, deep knots accurately. They’re great for general muscle tension, but for stubborn trigger points, direct pressure with fingers, tennis balls, or dry needling is more effective.
Are trigger points dangerous?
No. Trigger points aren’t tumors or structural damage. They’re functional problems in muscle tissue. Left untreated, they cause chronic pain and reduced mobility, but they don’t lead to serious illness. The danger lies in misdiagnosis-delaying treatment for something like a pinched nerve or heart condition because pain is assumed to be muscular.
What’s the best way to prevent trigger points?
Stay active, move often, and stretch daily. Avoid prolonged static postures-especially slouching or cradling your phone between your ear and shoulder. Keep your workspace ergonomic. Address stress through breathing or movement. And if you’ve had a past injury like whiplash or a fall, get checked for trigger points even if you feel fine now.


Anna Roh
December 10, 2025 AT 10:38Ugh, another one of those 'press on it until it stops hurting' articles. I've been doing the tennis ball thing for months. It helps for like 20 minutes, then my neck feels worse. Like... why is this even a thing?
Also, vitamin D? Really? I take 5000 IU daily and still feel like a ragdoll.
Rich Paul
December 11, 2025 AT 18:52lol u think u r the first person to find trigger points? bro this is just myofascial trigger point syndrome, which is a subset of myofascial pain syndrome, which is often comorbid with central sensitization syndromes like fibro and CFS. the real issue is neuromuscular dysregulation from chronic low-grade inflammation and glutamate excitotoxicity.
also dry needling > foam rolling any day, but only if the practitioner knows their anatomical landmarks. most PTs are just winging it with a needle.
ps: vitamin d deficiency is a confounder, not a cause. stop blaming your diet.
Delaine Kiara
December 12, 2025 AT 19:36MY FATHER HAD THIS. HE WENT TO 17 DOCTORS. ONE SAID IT WAS STRESS. ANOTHER SAID IT WAS A TUMOR. THE 18TH SAID 'IT'S JUST YOUR MUSCLES BEING DUMB.'
HE STARTED USING A LACROSSE BALL ON HIS TRAPS AT 4 AM EVERY DAY. HE CRIED. HE SCREAMED. HE WENT TO A CHIROPRACTOR WHO DIDN'T BELIEVE IN HIM.
THEN ONE DAY - HE WASN'T HURTING.
HE SAID IT FELT LIKE HIS MUSCLES WERE UNFOLDING LIKE A FLOWER.
I CRIED WHEN HE TOLD ME.
YOU GUYS. THIS IS REAL.
JUST PRESS.
AND DON'T STOP.
Ruth Witte
December 13, 2025 AT 21:22OMG YES THIS IS SO TRUE!! 🙌 I had migraines for 5 years and no one could figure it out. Then I found a knot the size of a marble under my jaw and pressed it for 90 seconds... and the headache just... vanished. Like, poof. 💥
Now I roll with a tennis ball every night before bed. It’s my new yoga. 🧘♀️💖
Also vitamin D - I was at 14 ng/mL. Took supplements. My pain dropped 70%. I’m not even joking. This is life-changing stuff!!
Katherine Rodgers
December 14, 2025 AT 07:47oh wow. so the answer to chronic pain is... buying a tennis ball? genius. next you’ll tell me the cure for cancer is lemon juice and yoga.
and let me guess - the author’s website has a $97 ‘trigger point masterclass’ and a $29.99 ‘myofascial release pillow’?
convenient.
also, dry needling? sure, let’s stick needles into our muscles because why not. no regulation, no oversight, just some guy who watched a YouTube video and now calls himself a ‘dry needling specialist.’
we’re all just one bad needle job away from permanent nerve damage.
thanks for the fearmongering, doc.
Lauren Dare
December 14, 2025 AT 12:29Interesting that you mention ‘misdiagnosis rates’ without citing the study. 57%? Which journal? What sample size? What diagnostic criteria?
Also, ‘trigger points don’t show up on imaging’ - true. But neither do anxiety, depression, or chronic stress. That doesn’t mean they’re not real. Or that they don’t need proper clinical evaluation.
There’s a difference between ‘this is underdiagnosed’ and ‘this is the only explanation.’
Also - vitamin D? 60% higher risk? Correlation ≠ causation. You’re conflating biomarkers with etiology.
Just saying - please cite your sources. Or at least don’t sound like a wellness influencer.
Gilbert Lacasandile
December 15, 2025 AT 09:47Hey, I just wanted to say this was super helpful. I’ve been dealing with shoulder pain for over a year and thought it was rotator cuff. Turns out it was a knot in my levator scapulae. I’ve been doing the tennis ball thing for a week now - it’s not magic, but it’s better.
Also, the posture tips? Game changer. I set a timer and now I do 3 shoulder rolls every 30 minutes. Feels like a tiny reset button.
Thanks for writing this. I wish more people knew about this stuff.
Lola Bchoudi
December 16, 2025 AT 01:40Great breakdown! Just to add - when doing ischemic compression, aim for 60-70% discomfort, not 100%. If you’re gritting your teeth and holding your breath, you’re activating the sympathetic nervous system, which keeps the muscle locked. Breathe out slowly as you press - it signals the muscle to release.
Also, combine with diaphragmatic breathing for 2 minutes after each session. Helps with vagal tone and reduces overall tension.
And yes - vitamin D matters. But so does magnesium glycinate. Low Mg = sustained muscle contraction. Supplementing helped my trigger points respond faster to pressure. Just a thought.
Morgan Tait
December 17, 2025 AT 18:41you know what’s really happening here? it’s all part of the pharmaceutical-industrial complex. they don’t want you to know you can fix this with a tennis ball because then people stop buying painkillers, botox injections, nerve blocks, and spinal stimulators.
and don’t get me started on the FDA - they banned myofascial release therapy in 1987 because it threatened Big Pharma’s monopoly on pain management.
they call it ‘trigger points’ so you think it’s some new fad. it’s ancient. chinese medicine knew this 3000 years ago. they called it ‘qi stagnation.’
they’re hiding the truth. but you? you’re awake now.
share this. save someone.
Darcie Streeter-Oxland
December 18, 2025 AT 18:34While the article presents a coherent and clinically plausible framework for the management of myofascial pain syndrome, it lacks sufficient methodological rigour in its evidentiary claims. The cited percentages for treatment efficacy are not referenced, and the distinction between anecdotal and empirical outcomes remains blurred.
Furthermore, the conflation of trigger point therapy with general musculoskeletal wellness advice risks promoting oversimplification of a complex, multifactorial condition.
One is reminded of the 19th-century belief in ‘humoral imbalance’ as a universal etiology - a paradigm that, while intuitively appealing, ultimately impeded scientific progress.
Recommendation: Peer-reviewed citations required.
Taya Rtichsheva
December 20, 2025 AT 14:55lol i tried the tennis ball thing and it just made me mad. like, why is my body like this? why can't i just be normal?
also i think my dog has trigger points. he winces when i pet his shoulder. maybe he needs a ball too. 🐶
anyway i'm just here for the memes
Christian Landry
December 21, 2025 AT 15:21Hey, I just wanted to say I tried the spray and stretch thing last week with some ice pack + static stretch. It didn’t work at first, but then I realized I was stretching too fast. Took it slow, held each stretch 45 sec, and did it 3x/day. After 4 days, my jaw pain was gone. 🤯
Also - anyone else notice that trigger points get worse when you’re stressed? I’ve been doing box breathing (4-4-4-4) and it helps more than I thought. Just a thought. 👍