When you take a macrolide antibiotic like azithromycin or clarithromycin for a sinus infection or bronchitis, you’re probably not thinking about your heart. But for some people, these common drugs can trigger a dangerous change in heart rhythm - a condition called QT prolongation - that can lead to a life-threatening arrhythmia known as Torsades de pointes. This isn’t theoretical. It’s documented, studied, and tracked by the FDA, the American Heart Association, and hospitals worldwide.
What Exactly Is QT Prolongation?
Your heart beats because of electrical signals that travel through muscle tissue. The QT interval on an ECG measures how long it takes for your heart’s lower chambers (ventricles) to recharge between beats. When this interval gets too long, the heart’s electrical system becomes unstable. That’s QT prolongation. It doesn’t cause symptoms on its own, but it sets the stage for Torsades de pointes - a rapid, irregular heartbeat that can turn into cardiac arrest if not caught quickly. Macrolide antibiotics interfere with a specific potassium channel in heart cells called the hERG channel. This channel helps reset the heart’s electrical charge after each beat. When macrolides block it, the reset takes longer. That’s what stretches out the QT interval. It’s not a glitch - it’s a direct, measurable effect on heart muscle physiology.Not All Macrolides Are the Same
Many people assume all macrolides are equally risky. They’re not. There’s a clear hierarchy of danger:- Clarithromycin - Highest risk. It doesn’t just block potassium channels; it also shuts down a liver enzyme (CYP3A4) that breaks down other drugs. This means if you’re taking another medication that affects your heart rhythm - say, a statin or an antifungal - clarithromycin can cause those drugs to build up to toxic levels. It carries a black box warning from the FDA.
- Erythromycin - Moderate risk. It’s less potent at blocking potassium channels than clarithromycin, but it causes severe nausea and vomiting in many people. That can drop your potassium levels, which further increases arrhythmia risk.
- Azithromycin - Lowest risk among macrolides, but still risky. It doesn’t interfere much with liver enzymes, and its effect on potassium channels is weaker. But here’s the catch: even azithromycin has been linked to sudden cardiac death in large population studies. A 2012 study of over 1.3 million people found it raised the risk of heart-related death by nearly 3 times compared to amoxicillin - especially in the first five days of use.
Who’s Most at Risk?
The good news? For most healthy adults, the risk is very low. The bad news? For certain groups, it’s not just low - it’s dangerous. Six key factors raise your risk dramatically:- Being female - Women make up nearly 7 out of 10 cases of macrolide-induced Torsades.
- Age over 65 - Your heart’s electrical system slows with age. Risk doubles.
- Already having a long QT interval - If your baseline QTc is above 450 ms (in men) or 470 ms (in women), you’re already on thin ice. Adding a macrolide can push you over the edge.
- Taking other QT-prolonging drugs - Antidepressants, antifungals, anti-nausea meds, and even some antihistamines can stack with macrolides. Each extra drug increases risk by almost 80%.
- Low potassium or magnesium - Dehydration, diuretics, or eating disorders can drop your electrolytes. Hypokalemia triples your risk.
- Heart failure or structural heart disease - If your heart is already damaged, even small electrical changes can trigger chaos. Risk increases more than fivefold.
What Doctors Are Doing About It
In 2020, the American Heart Association officially labeled clarithromycin, erythromycin, and azithromycin as drugs with a known risk of Torsades. Since then, prescribing patterns have shifted.- Clarithromycin prescriptions dropped by over 23% in Medicare patients between 2020 and 2021.
- Guidelines now recommend avoiding all macrolides in patients with a history of Torsades or congenital long QT syndrome.
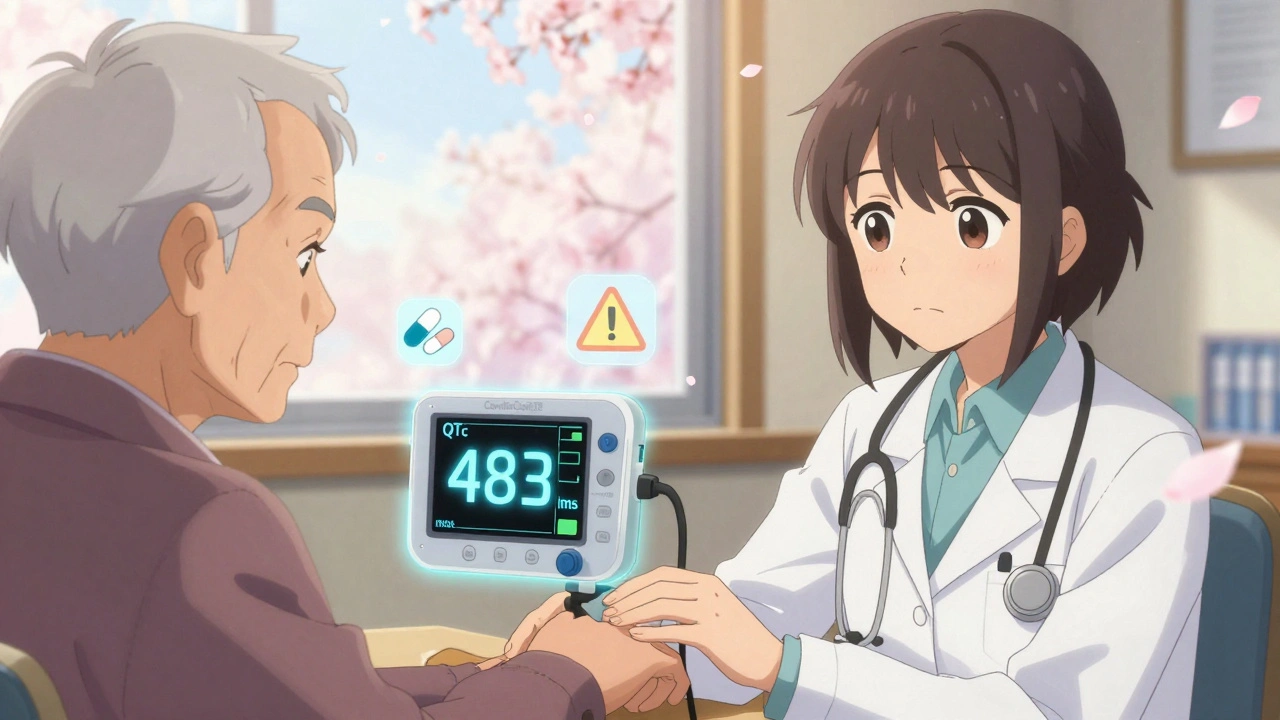
- If you’re over 65, have heart disease, or take other heart-affecting drugs, your doctor should check your ECG before prescribing a macrolide.
- If your QTc goes above 470 ms (men) or 480 ms (women), or increases by more than 60 ms from baseline, the drug should be stopped immediately.
Real-World Evidence: What the Data Shows
A 2023 study in Frontiers in Cardiovascular Medicine analyzed over 500 cases of drug-induced Torsades. Macrolides were the third most common cause - behind antiarrhythmics and antipsychotics. Even more telling: 18% of those cases involved azithromycin, despite its reputation as the “safest” macrolide. During the COVID-19 pandemic, azithromycin was given with hydroxychloroquine to hundreds of thousands of patients. The combination caused an average QTc increase of 26.2 milliseconds - enough to push many into dangerous territory. The FDA had to issue emergency warnings. And here’s something few patients know: the risk isn’t just about the dose. It’s about timing. The highest risk window is the first 5 days of treatment - right when people feel like they’re getting better. That’s when sudden cardiac deaths spike.New Tools to Help Manage the Risk
Technology is catching up. In 2023, the FDA approved the CardioCare QT Monitor, a handheld ECG device that gives accurate QTc readings in under 30 seconds. Some urgent care clinics and pharmacies now use it before dispensing macrolides to high-risk patients. A more advanced tool is the Macrolide Arrhythmia Risk Calculator (MARC), developed at Brigham and Women’s Hospital. It takes into account age, sex, kidney function, current medications, electrolyte levels, and even genetic markers. It predicts individual TdP risk with 89% accuracy. Doctors in major U.S. hospitals are starting to use it - but it’s not yet standard everywhere.What Should You Do?
If you’re prescribed a macrolide:- Ask: “Is this the best choice for me, or is there a safer alternative?”
- Tell your doctor about every other medication you take - even over-the-counter ones.
- Ask if you need an ECG before starting the drug, especially if you’re over 65, female, or have heart problems.
- Watch for symptoms: dizziness, fainting, palpitations, or sudden shortness of breath. If you feel any of these, stop the drug and seek help.
- Don’t skip follow-up blood tests. Low potassium is easy to fix - but deadly if ignored.
The Bottom Line
Macrolide antibiotics save lives. But they’re not harmless. Their cardiac risk is real, measurable, and preventable. The key isn’t avoiding them entirely - it’s using them wisely. For most people, the benefits outweigh the risks. But if you have even one risk factor, you need to be proactive. Your doctor isn’t always thinking about your heart when they write a prescription for azithromycin. You have to be.Can azithromycin really cause a heart attack?
Azithromycin doesn’t directly cause heart attacks, but it can trigger a dangerous heart rhythm called Torsades de pointes, which can lead to sudden cardiac arrest - a type of sudden death that looks like a heart attack. This is rare in healthy people but significantly more likely if you have other risk factors like heart disease, low potassium, or are taking other QT-prolonging drugs.
Is clarithromycin safer than erythromycin?
No. Clarithromycin is actually riskier than erythromycin. It blocks potassium channels more strongly and also interferes with liver enzymes that break down other medications, which can cause dangerous drug buildups. Erythromycin is more likely to cause vomiting, which lowers potassium and adds to the risk - but clarithromycin has a higher overall arrhythmia potential. That’s why clarithromycin carries a black box warning from the FDA.
Should I get an ECG before taking a macrolide antibiotic?
If you’re over 65, female, have heart disease, take other heart-affecting medications, or have a history of fainting or irregular heartbeat - yes. Guidelines recommend a baseline ECG for anyone with two or more risk factors. Even if you feel fine, a hidden heart rhythm issue could be triggered by the drug.
What are the signs that a macrolide is affecting my heart?
You might feel dizzy, lightheaded, or like you’re about to pass out. Some people report heart palpitations - a fluttering, racing, or skipping sensation in the chest. Others have sudden shortness of breath or fainting. These symptoms can appear within hours or days of starting the drug. If you experience any of them, stop taking the medication and get medical help immediately.
Can I take azithromycin if I’m on a statin?
It’s risky. Azithromycin doesn’t strongly interfere with statin metabolism like clarithromycin does, so the interaction is less severe. But both drugs can prolong the QT interval. If you’re on a statin and have other risk factors - like high blood pressure, diabetes, or kidney disease - your doctor should check your ECG before prescribing azithromycin. Safer alternatives like doxycycline are often preferred in these cases.
Are there any new macrolide antibiotics without this risk?
Researchers have been trying to develop “cardiosafe” macrolides. One called solithromycin showed 78% less potassium channel blockade than clarithromycin in trials. But its development was stopped in 2022 due to liver toxicity. No new macrolide has been approved since then that fully eliminates the QT risk. Until then, the existing drugs - with their known profiles - remain the standard.

Katherine Liu-Bevan
December 10, 2025 AT 15:26Just had my grandma hospitalized last year after a simple azithromycin script for bronchitis. She’s 72, on a statin, and had a baseline QTc of 465. No symptoms before. After three days, she collapsed walking to the kitchen. ECG showed Torsades. They reversed it, but she’s been on a pacemaker since. This isn’t theoretical-it’s happening to people we know. Always ask for an ECG if you’re over 65 or on multiple meds.
Courtney Blake
December 10, 2025 AT 21:14Of course the FDA cares about heart rhythms but not about the 500,000 people who die from untreated sinus infections every year because doctors are too scared to prescribe antibiotics. You want to live in a world where every pill comes with a 12-page warning label? Good luck surviving a cold.
Lisa Stringfellow
December 12, 2025 AT 20:44So let me get this straight-you’re telling me that after 30 years of prescribing azithromycin, doctors just now figured out it might be dangerous? And now they want us to get ECGs before every antibiotic? That’s not medicine, that’s insurance-driven fearmongering. My cousin took it for pneumonia in ‘09 and lived to 40. Coincidence?
Kristi Pope
December 13, 2025 AT 08:49Thank you for writing this with such clarity. I’m a nurse and I’ve seen too many patients assume ‘it’s just an antibiotic’-like it’s a vitamin. But your breakdown of risk factors? Gold. I now have a printed checklist I hand out to anyone over 60 on multiple meds. One woman came back saying her daughter got tested for long QT after reading this. That’s the ripple effect we need.
Eddie Bennett
December 14, 2025 AT 00:31My dad’s a cardiologist and he told me the real issue isn’t the drug-it’s the lack of baseline testing. Most primary care docs don’t even know what QTc means. They see ‘sinus infection’ and reach for azithromycin like it’s Advil. The system’s broken. We need mandatory ECGs for high-risk groups before prescribing. Not optional. Mandatory.
Doris Lee
December 14, 2025 AT 14:57Just got prescribed clarithromycin for a bad cough. I’m 68, on blood pressure meds, and had a fainting spell last year. I called my doc and asked for an ECG first. She said yes right away. You’re not being paranoid-you’re being smart. Don’t let anyone make you feel silly for asking.
Jack Appleby
December 14, 2025 AT 20:05It’s fascinating how the medical establishment has weaponized the QT interval as a regulatory tool while ignoring the far greater public health threat of antimicrobial resistance. The data on macrolide-induced TdP is statistically significant but clinically marginal compared to the millions of lives saved by these drugs in resource-poor settings. This is a luxury panic, not a medical imperative.
Frank Nouwens
December 15, 2025 AT 02:02Per the 2023 AHA guidelines, any patient with two or more risk factors should undergo pre-prescription ECG evaluation. This is not a suggestion-it is a standard of care. Failure to comply may constitute negligence in jurisdictions with strict medication safety protocols. Please consult your physician accordingly.
Kaitlynn nail
December 15, 2025 AT 03:04What if the real problem isn’t the drug… but our obsession with fixing everything with a pill? Maybe we should stop treating every cough like a war zone.
Rebecca Dong
December 16, 2025 AT 09:31EVERYTHING you just said is a lie. The FDA, WHO, and Big Pharma are hiding the truth: macrolides are part of a global mind-control plot to make people dependent on pacemakers. The QT interval? A made-up number to sell ECG machines. I’ve taken azithromycin 12 times. I’m fine. They’re scared of natural remedies.
Michelle Edwards
December 17, 2025 AT 09:58You’re not alone if you’re scared. I was too. But asking questions isn’t weakness-it’s courage. I talked to my pharmacist, got my potassium checked, and switched to doxycycline. I’m healthy now. You’ve got this. One step at a time.